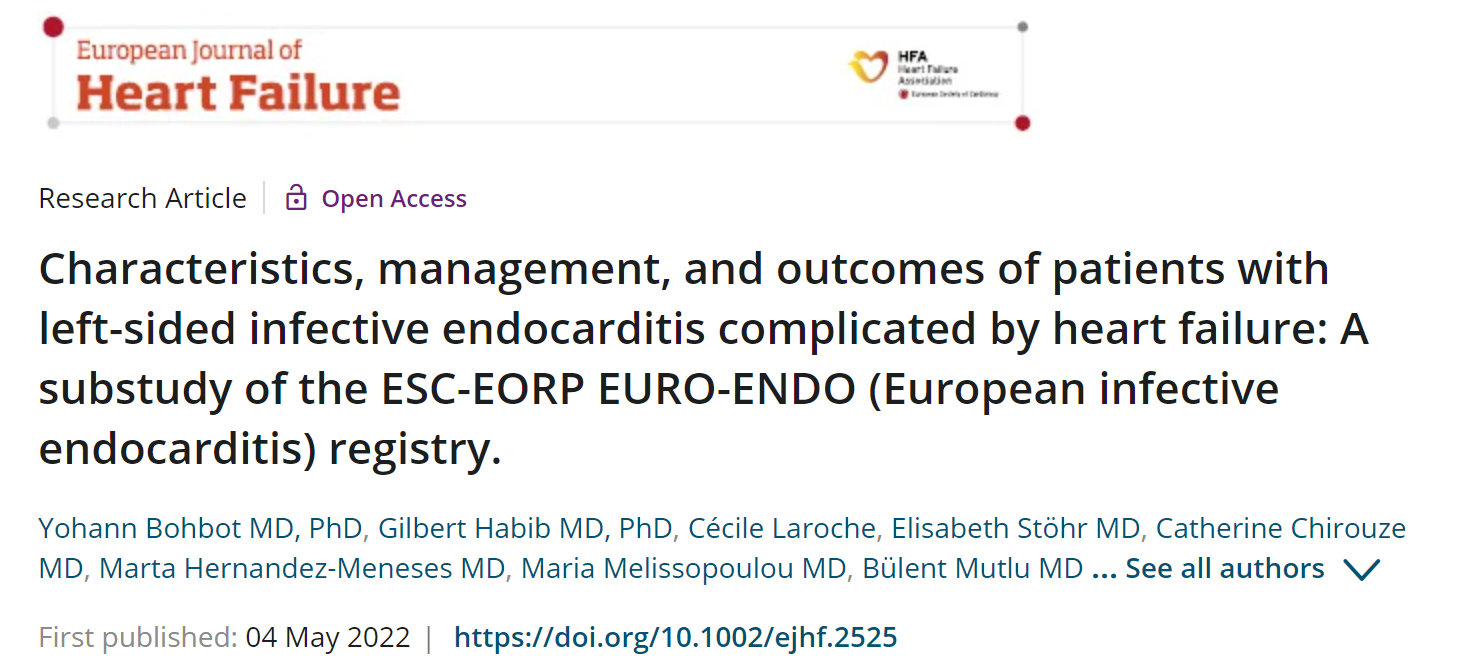
Eur J Heart Fail:伴有心衰的左侧感染性心内膜炎患者特征、治疗和结局情况
2022-05-08 MedSci原创 MedSci原创
CHF常见于左侧IE,且与年龄较大、合并症较多、病变较晚期,以及与较高的30天和1年死亡率显著相关。早期手术与较低的死亡率密切相关,但只有大约一半的CHF患者接收了手术治疗。
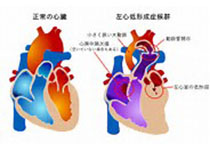
尽管感染性心内膜炎(IE)在诊断、抗感染和手术治疗方面取得了重大进展,但它仍然是一种致命性的疾病。充血性心力衰竭(CHF)是影响瓣膜和人工瓣膜性IE预后的一个重要因素,也是早期手术的主要适应症之一。大约10年前,两项研究报道CHF患者中IE很常见,是住院和1年死亡率的独立预测因子,尽管早期手术与降低这些患者的死亡率独立相关,但只有大约50%到60%的病例接收了手术治疗。
近日,心血管领域权威杂志European Journal of Heart Failure上发表了一篇研究文章,研究人员旨在评估ESC-EORP欧洲心内膜炎(EURO-ENDO)登记中心内左侧感染性心内膜炎(IE)合并充血性心力衰竭(CHF)患者的当前治疗和生存情况。
在这个前瞻性登记的3116例患者中,2449例(平均年龄为60岁,69%为男性)患有左侧(自然或人工)IE的患者被纳入研究。CHF患者(n=698,28.5%)较无CHF患者年龄大,有更多的合并症和更严重的瓣膜损伤(主动脉弓受累、赘生物>10mm、严重返流/人工瓣膜裂开)(均p≤0.019)。伴有IE的CHF患者30天和一年的死亡率高于那些没有IE的CHF患者(分别为20.5%和9.0%、36.1%和19.3%),CHF仍与30天(OR为95%CI=2.37(1.73-3.24),p<0.001)和一年(HR和95%CI=1.69(1.40-2.05),p<0.001)的死亡率密切相关,即使在已知的结局预测因子被调整或在年龄、性别和合并症进行倾向匹配后(两组n=618[88.5%],均p<0.001)。
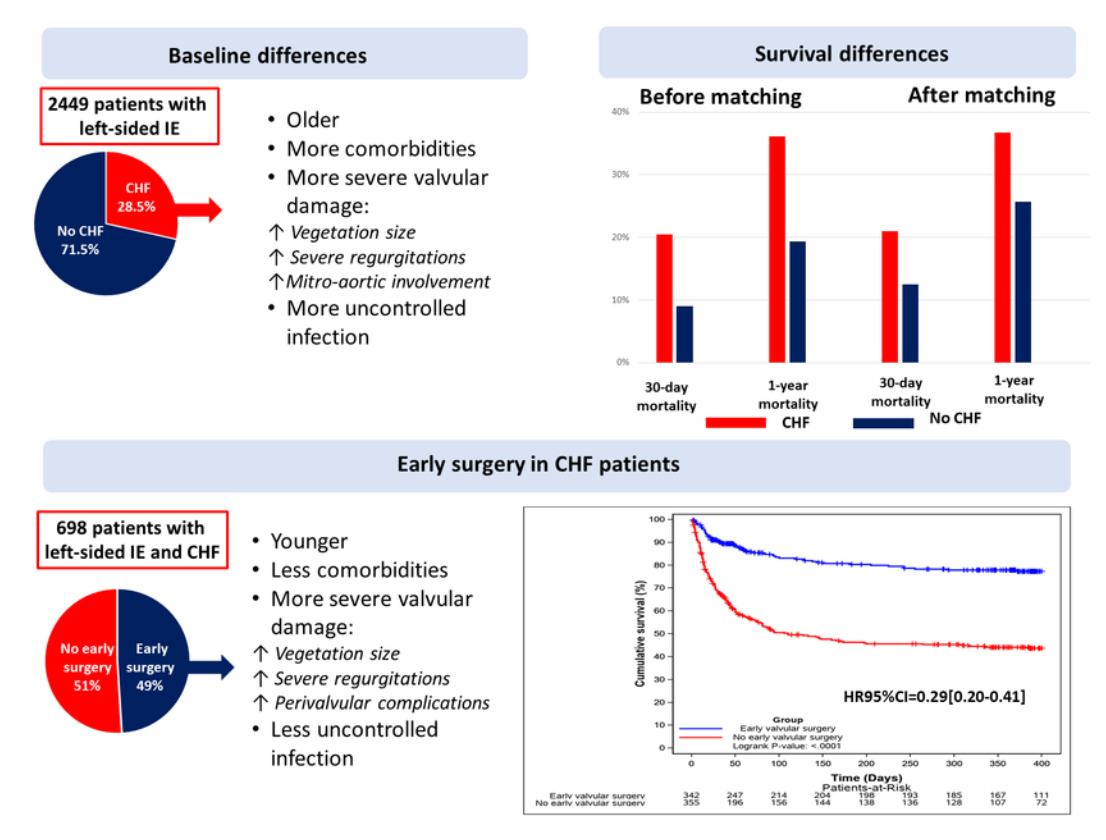
49%伴有CHF的IE患者进行了早期手术,在调整了年龄、性别、Charlson指数、脑血管意外、金黄色葡萄球菌IE、链球菌IE、未控制的感染、赘生物大小>10mm、严重瓣膜返流和/或新的人工瓣膜破裂、瓣膜周围并发症和人工瓣膜IE后,通过多变量分析,仍与30天(OR为95%CI=0.22[0.12-0.38];p<0.001)和1年(HR为95%CI=0.29[0.20-0.41];p<0.001)死亡率的大幅降低相关。
由此可见,CHF常见于左侧IE,且与年龄较大、合并症较多、病变较晚期,以及与较高的30天和1年死亡率显著相关。早期手术与较低的死亡率密切相关,但只有大约一半的CHF患者接收了手术治疗,主要是因为手术风险而未手术。
原始出处:
Yohann Bohbot.et al.Characteristics, management, and outcomes of patients with left-sided infective endocarditis complicated by heart failure: A substudy of the ESC-EORP EURO-ENDO (European infective endocarditis) registry.European journal of heart failure.2022.https://onlinelibrary.wiley.com/doi/abs/10.1002/ejhf.2525
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#内膜#
48
#感染性#
52
合并心衰的IE也应该闯手术,获益大于风险
45
#心内膜炎#
56
#ART#
46
#HEART#
36
#患者特征#
33