PNAS:他汀类药物使癌细胞无法吸收蛋白而“饿死”
2020-03-17 于晓程 生物探索
流行病学迹象表明,长期服用他汀类药物的人,往往很少患有侵袭性癌症。在美国,每天有超过3500万人服用这类药物来降低血液胆固醇水平。美国约翰霍普金斯大学医学院的研究人员在对人体细胞进行的实验中,发现越来
流行病学迹象表明,长期服用他汀类药物的人,往往很少患有侵袭性癌症。在美国,每天有超过3500万人服用这类药物来降低血液胆固醇水平。美国约翰霍普金斯大学医学院的研究人员在对人体细胞进行的实验中,发现越来越多的证据证明这种无处不在的药物可能杀死癌细胞,并揭示了它们如何发挥作用的线索。这项新研究的结果发表在的《PNAS》上。
Devreotes教授及其团队通过对FDA批准的约2500种药物的无偏筛选开始了这项新研究,目的是查看哪种药物对经基因改造的癌症基因PTEN突变的细胞杀灭率最高,该基因编码抑制肿瘤生长的酶。结果发现,在成千上万种药物中,他汀类药物,尤其是匹伐他汀,成为杀灭癌症能力的最高竞争者。
然后,研究人员研究了他汀类药物可能影响的分子途径,他汀类药物除了可以阻断产生胆固醇的肝酶之外,还可以阻止小分子香叶基香叶基焦磷酸(GGPP)的产生,该小分子负责将细胞蛋白连接至细胞膜。当研究人员将匹伐他汀和GGPP加入具有PTEN突变的人类癌细胞中时,发现GGPP阻止了他汀的杀伤作用并且癌细胞得以存活,这表明GGPP可能是癌细胞存活的关键因素。
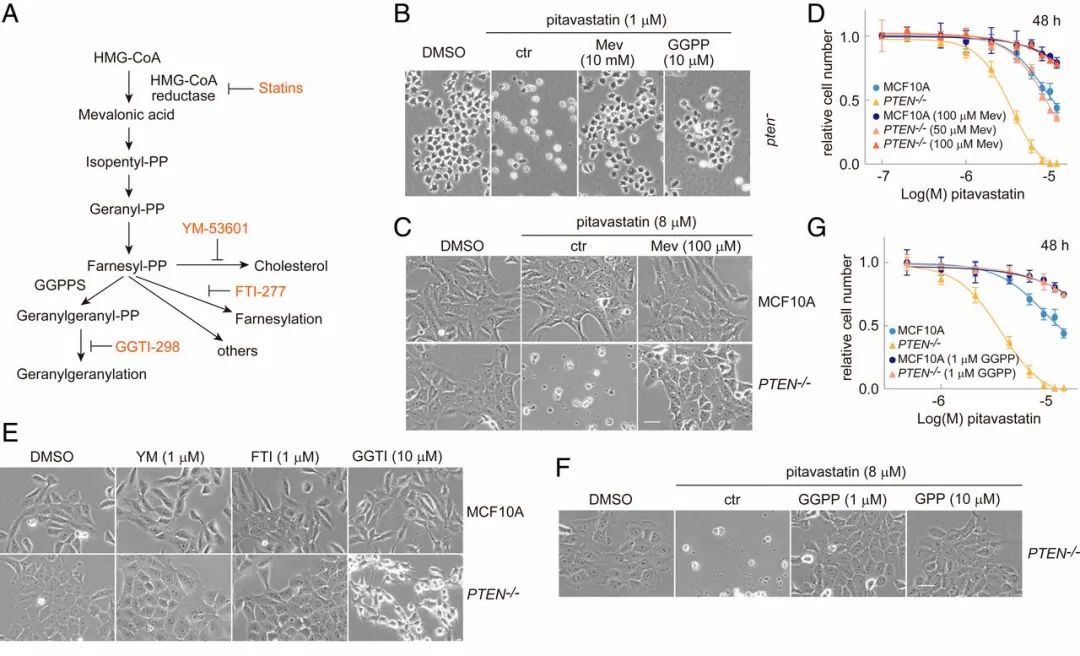
香叶酰香叶酰化的调节介导了匹伐他汀的细胞毒性作用
接下来,在显微镜下观察经改造缺乏制造GGPP酶的细胞,研究人员发现,当细胞开始死亡时就停止了移动。正常情况下,癌细胞是一堆移动的能量,需要消耗大量营养物质来维持其不受控制的生长。研究人员怀疑静止的癌细胞“饿死了”,于是通过在细胞环境中的蛋白质上添加荧光标记来测量他汀类药物处理过的细胞的摄入量。无论是否添加他汀类药物,正常细胞都带有荧光标记,表明它们从周围环境中摄取蛋白质;但是,具有PTEN突变的癌细胞在添加他汀类药物后,几乎不吸收任何发光蛋白,他汀类药物治疗的癌细胞无法吸收蛋白质,从而导致其饥饿。
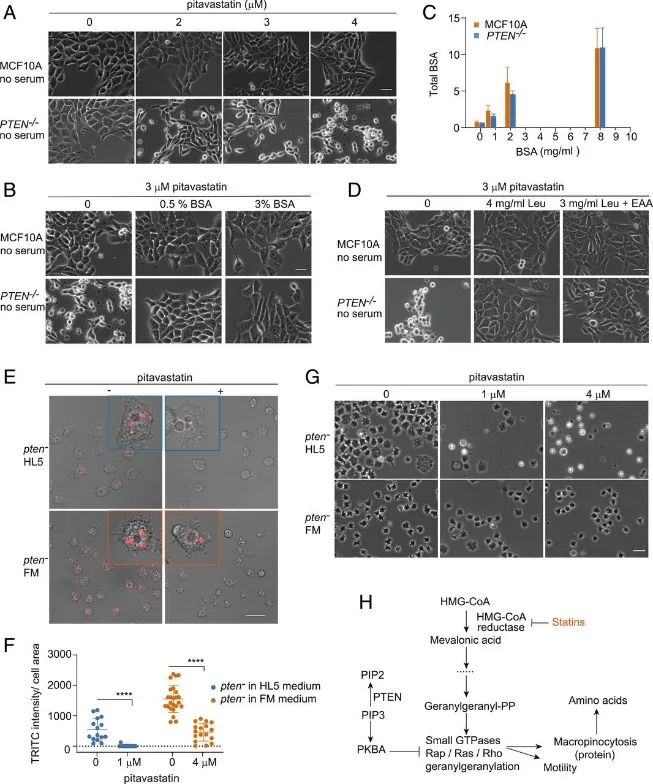
匹伐他汀引起大胞饮缺陷会导致PTEN−/−细胞的蛋白质和氨基酸饥饿
研究人员说,这些发现增加了先前研究的证据,他汀类药物在对抗某些形式的癌症方面可能是有价值的,该团队下一步计划是研究他汀类药物对癌症患者和阻断GGPP的化合物的影响。
原始出处:
Zhihua Jiao, et al. Statin-induced GGPP depletion blocks macropinocytosis and starves cells with oncogenic defects. PNAS.February 25, 2020 117
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PNAS#
32
#他汀类药#
27
#癌细胞#
26
有意思学习了
81
学习了,学习了
92