J Bone Oncol:诊断时有骨转移的小细胞肺癌患者的临床结局
2020-04-23 MedSci原创 MedSci原创
小细胞肺癌(SCLC)患者初诊时有骨转移的小细胞肺癌(SCLC)患者的特点和预后因素几乎没有报道。本研究旨在分析这些患者的预后因素,建立生存评分系统,为临床治疗决策提供依据。
小细胞肺癌(SCLC)患者初诊时有骨转移的小细胞肺癌(SCLC)患者的特点和预后因素几乎没有报道。本研究旨在分析这些患者的预后因素,建立生存评分系统,为临床治疗决策提供依据。
回顾性分析2010年5月至2015年5月在我院就诊的102例SCLC骨转移患者的诊断。对数秩检验和多因素Cox回归分析用于评估生存的潜在临床预测指标。基于重要的独立预后因素的危险比,开发了评分系统。
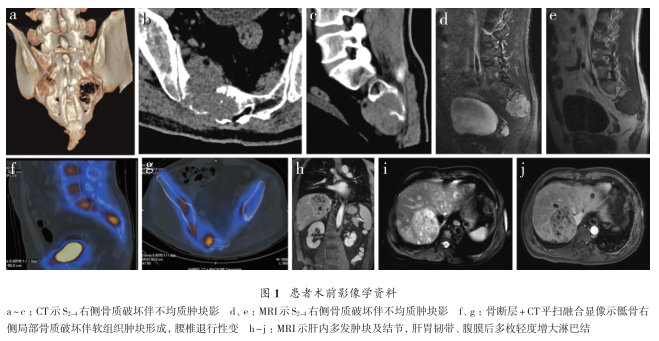
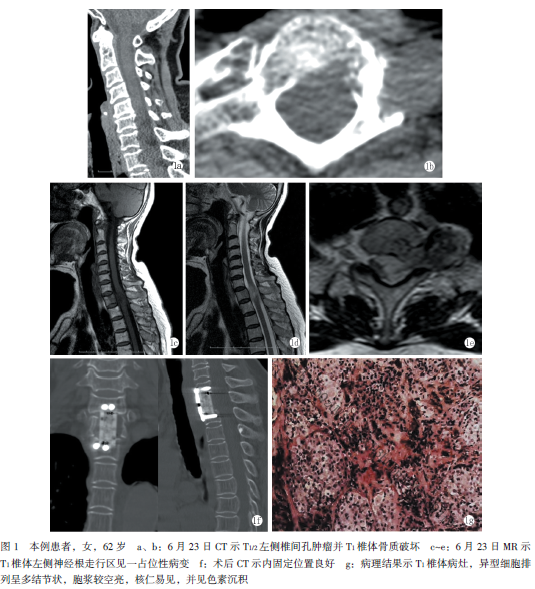
结果显示,骨转移最常见的部位是脊柱(64.7%),并且26位患者(25.6%)发生了单一骨转移。中位生存期为10.4个月,两年生存率为10.3%。年龄,骨转移的数量和骨外远处转移的发生是整体生存的重要独立预后因素。根据评分,将患者分为三组。三组患者的中位生存时间分别为6.4个月,8.5个月和12.4个月,两年生存率分别为0%,2.9%和19.3%(p = 0.000)。26位患者(25.5%)发生了骨骼相关事件(SRE),最常见的SRE是放射至骨骼(22.5%)和脊髓受压(11.8%)。
综上所述,该研究包括诊断时患有骨转移的SCLC患者的初步临床数据,需要进行更多研究。
原始出处:
Linlin Gong, Liming Xu, et al., Clinical outcome for small cell lung cancer patients with bone metastases at the time of diagnosis. J Bone Oncol. 2019 Dec; 19: 100265.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肺癌患者#
37
#Oncol#
27
#临床结局#
38
#Bone#
35
系统,为临床治疗决策提供依据。
0
谢谢梅斯分享这么多精彩信息
59