Cardiovasc Diabetol:血糖变异性与颈动脉的内膜-中膜厚度和组织特征的相关性
2021-05-09 MedSci原创 MedSci原创
在没有心血管疾病的2型糖尿病患者中,连续的血糖监测评估的血糖变异性与颈动脉壁的组织特征有关
血糖变异性与动脉粥样硬化进展之间的关联尚不完全清楚。本研究旨在评估血糖变异性与早期阶段动脉粥样硬化进展的相关性。
注释:血糖变异性(GV):以平均血糖为基准的血糖波动,包括从波峰到波谷的振幅、频率、持续时间等。
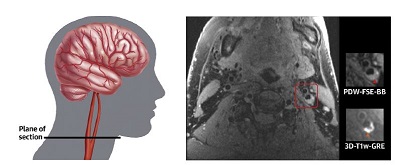
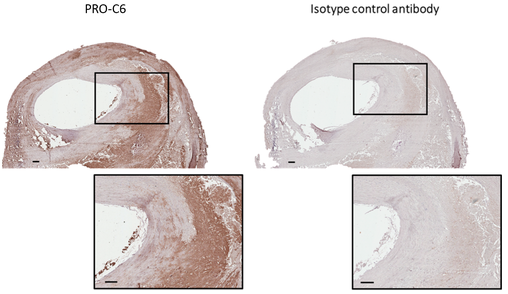
研究人员进行了一项横断面分析,对受试者的血糖进行持续监测,同时检测了他们颈动脉的内膜中层厚度(IMT)和灰度中值(GSM)。研究人员使用了基于医院的多中心前瞻性观察队列研究的基线数据,该基线研究针对的是30-80岁的无心血管疾病史的日本2型糖尿病患者。采用Freestyle Libre Pro进行连续血糖监测,每15分钟测一次血糖(最多八天),用于计算血糖变异性指标。
注释:IMT系指颈动脉内膜管腔面与外膜分界面之间的距离。临床上通过彩色多普勒超声诊断仪检查颈动脉内膜中层厚度(IMT)来确定是不是有动脉粥样硬化斑块形成。GSM表示组织特征。
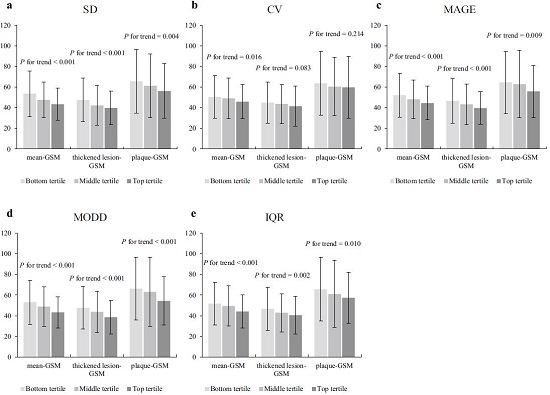
血糖变异性与IMT的相关性
共纳入了600位受试者(年龄 64.9±9.2岁,63.2%的男性,HbA1c 7.0±0.8%),日间和一日内葡萄糖变异性较大的受试者的GSM较低,并且这些关联中的大多数在统计学上均具有显着性。IMT未见存在基于血糖变异性而不同的趋势。
血糖变异性与GSM的相关性
经常规心血管危险因素(包括HbA1c)调整后,血糖标准差(回归系数β=-5.822; 95% CI -8.875~-2.768, P<0.001)、血糖变异系数(β=-0.418;-0.685~-0.151, P=0.002)、血糖漂移平均振幅(β=-1.689; -2.567~-0.811, P<0.001)、每日差异平均值(β=-6.500; -9.758~-3.241, P<0.001)和四分位范围(β=-4.289; -6.964~-1.614, P=0.002)与平均-GSM之间存在统计学意义上的相关性。没有任何血糖变异性指标与IMT有统计学意义的关联。
总之,在没有心血管疾病的2型糖尿病患者中,连续的血糖监测评估的血糖变异性与颈动脉壁的组织特征有关。
原始出处:
Taya Naohiro,Katakami Naoto,Mita Tomoya et al. Associations of continuous glucose monitoring-assessed glucose variability with intima-media thickness and ultrasonic tissue characteristics of the carotid arteries: a cross-sectional analysis in patients with type 2 diabetes. Cardiovasc Diabetol, 2021, 20: 95. https://doi.org/10.1186/s12933-021-01288-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#BET#
36
#ASC#
27
#内膜#
23
#DIA#
26
#相关性#
38
#颈动脉#
26
#血糖变异#
39
#变异#
33
长见识了
65
好文章!
64