Neurology:独立于传统血管危险因素,循环白细胞介素-6(IL-6)水平与发生缺血性卒中长期风险呈正线性相关!
2022-01-16 Naomi MedSci原创
近日,研究人员利用已发表/未发表研究进行系统回顾和荟萃分析,探索基于人群的前瞻性队列研究中循环IL-6水平与缺血性卒中发病风险的关系,证实了较高的IL-6水平与较高的发生缺血性卒中长期风险呈线性关系。
卒中是世界范围内成年人残疾和死亡的主要原因。确定卒中的危险因素对于制定有效的一级和二级预防策略非常重要。炎症最近作为降低缺血性卒卒中险的一个潜在目标引起了人们的关注。来自大规模试验的数据提供了部分证据,证明抗炎治疗可以降低心血管疾病的风险。尽管如此,这些试验测试了心血管事件终点和关于专门用于预防卒中的抗炎方法的有效证据很少。
开发有效的抗炎治疗途径以预防卒中将需要确定与卒中发病相关的关键炎症介质。虽然有大量文献表明炎症的一般标志物C-反应蛋白(CRP)水平与卒中的相关性,但关于其他炎症细胞因子的数据有限。来自人类遗传学研究的数据表明,促炎症细胞因子白细胞介素-6(IL-6)在血管疾病中的潜在致病作用,有望成为新药物靶点。
明确循环IL-6水平与缺血性卒中之间关联和相关机制,将推动IL-6信号的抗炎治疗的进一步迈进。虽然前瞻性队列研究已确定循环中IL-6水平与冠状动脉疾病风险之间存在明显的相关性,但表明与缺血性卒中关联的证据有限,还涉及动脉粥样硬化以外的机制。近日,有研究人员利用已发表文献的汇总数据以及未发表的队列研究进行系统回顾和荟萃分析,以探索基于人群的前瞻性队列研究中循环IL-6水平与缺血性卒中发病风险的关系。
遵循Prisma指南,研究人员系统地筛选了PubMed搜索引擎,从最初到2021年3月,进行基于人群的前瞻性队列研究,探索循环中IL-6水平与缺血性卒中发病风险之间的关系。将缺血性卒卒中险的关联估计与随机效应模型合并,并在剂量-反应荟萃分析中探索非线性效应。采用纽卡斯尔-渥太华量表(NOS)评估偏倚风险。使用漏斗图和修剪到填充的分析来评估出版偏倚。
- 确定了11项研究(27,411人; 2,669例卒中事件)符合纳入标准。
- 平均年龄为60.5岁,女性占54.8% 。整体而言,纳入研究的质素较高(中位数为8/9,四分差为7至9)。
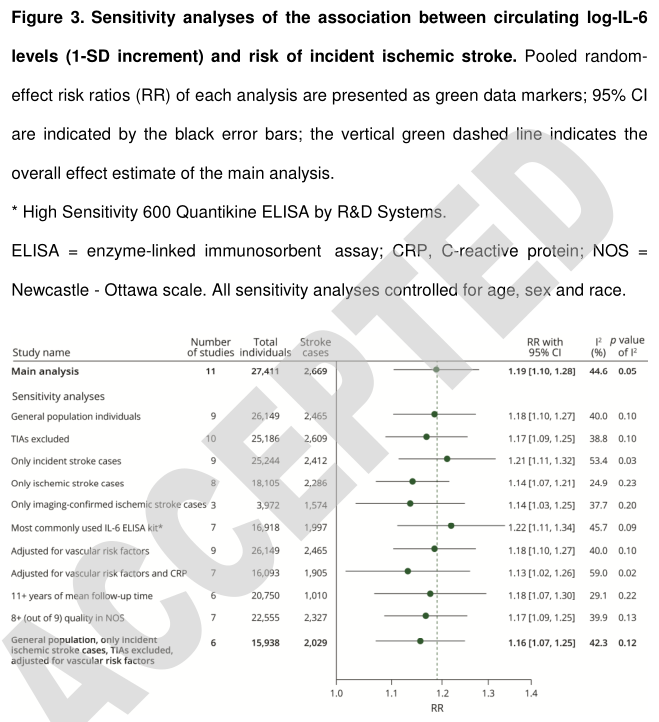
- 在荟萃分析中,循环对数转化IL-6水平的1个标准差增加与平均随访12.4年(RR 1.19; 95% CI 1.10-1.28)发生缺血性卒中的风险增加19% 相关。
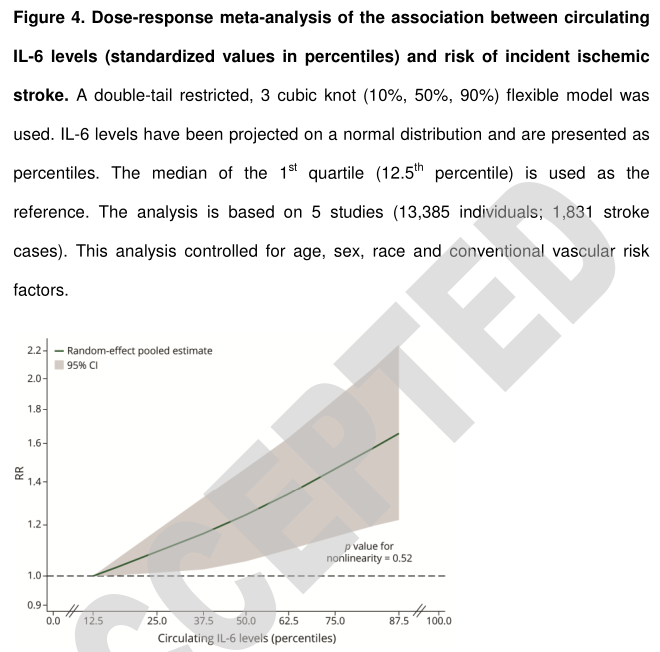
- 剂量-反应荟萃分析显示循环IL-6水平与缺血性卒中风险呈线性相关。
-
在限于低偏倚风险的研究和完全调整人口和血管风险因素的研究中,只有适度的异质性,敏感性分析的结果是一致的。
- 调整发表偏差后,结果也保持稳定。
在社区居民中,较高的循环IL-6水平与较高的发生缺血性卒中的长期风险呈线性关系,与传统的血管危险因素无关。结合基因研究和临床试验的发现,这些结果为IL-6信号在缺血性卒中中的关键作用提供了额外的支持。
文献来源:Papadopoulos A, Palaiopanos K, Björkbacka H, et al. Circulating Interleukin-6 Levels and Incident Ischemic Stroke: A Systematic Review and Meta-analysis of Prospective Studies [published online ahead of print, 2021 Dec 30]. Neurology. 2021;10.1212/WNL.0000000000013274. doi:10.1212/WNL.0000000000013274
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#缺血性卒#
28
#Neurol#
40
#缺血性#
31
#血管危险因素#
40
#IL-6#
57
#长期风险#
0
#白细胞介素#
43
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
69
学习了,以前只知道CRP。现在多了一种
72
学习了
68