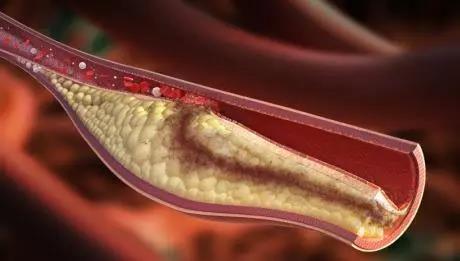
Hypertension:高血压前期进展为高血压的患者,左室肥厚风险更高
2019-03-09 国际循环编辑部 国际循环
近期,研究人员对PAMELA (Pressioni Monitorate E Loro Associazioni)处登记人群进行横断面和纵向数据分析,以评估左心室质量指数(LVMI)正常的亚组人群中入组时高血压前期和左心室肥厚(LVH)的关系以及相关的新发左室肥厚风险。最终研究结果发表于Hypertension杂志。基线状态下,横断面分析共纳入1397例超声心动图参数可测的未治疗患者。纵向分析则纳
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
45
#TENS#
34
#高血压前期#
0
#Hypertension#
32