Neurology:2017年和2010年修订的McDonald标准在预测临床孤立综合征后MS诊断中的表现
2021-10-30 Naomii MedSci原创
2017年McDonald标准相较于2010年McDonald标准,预测CDMS方面显示出更高的敏感性、更低的特异性、相似的准确性,且缩短MS的诊断时间,更准确区分了CIS术后早期患者CDMS。
2001年,MRI被正式纳入多发性硬化症(MS)诊断标准,以显示多发性硬化症病变的空间扩散(DIS)和时间扩散(DIT)。随后McDonald标准的更新简化了多发性硬化症的诊断,同时保持了敏感性、特异性和准确性。McDonald标准缩短了患有临床隔离综合征(CIS)的患者从出现症状到诊断MS的时间,而不需要等待第二次临床事件的发生。这一点至关重要,因为越来越多的治疗方法已经被证明在有利地改变MS病程方面是有效的,特别是在早期开始的情况下。
最近,关于MRI和CSF分析在多发性硬化症诊断中的应用的新证据已经出现。MAGNIMS网络在2016为DIS提出了修正的磁共振成像标准。这些循证建议的性能在一项大型的多中心MAGNIMS研究中进行了评估,该研究为2017年修订的MS诊断标准提供了信息,包括消除有症状和无症状病变之间的区别,以及在DIS中合并皮质和旁皮质病变(数据可从Dryad:表e-1 https://doi.org/10.5281/zenodo.5566178).获得。此外,在符合DIS标准的CIS患者中,脑脊液特异性寡克隆带(OCB)的存在可以在没有DIT的临床或磁共振证据的情况下诊断为MS(来自Dryad:Table e-1 https://doi.org/10.5281/zenodo.5566178).的数据)。MAGNIMS网络提出了一个额外的修改,以提高标准的特异性,但未包括在2017年修订中,即将建立脑室周围受累所需的病变数量从1个增加到3个。发表后,几项研究比较了2017年和2010年修订的McDonald标准在9-14岁的成年人和儿童CIS患者中的表现。全球范围内,他们显示2017年McDonald标准在预测临床明确(CD)MS方面比2010年的标准具有更高的敏感性,但特异性较低,但MS诊断时间更短。
与2017年修订的McDonald标准的表现相关的几个方面仍需充分评估。这些标准的表现主要是在CIS患者的小的、单中心性队列中进行评估的。使用了不同的结果,包括在相对较短或不同的随访后,或者通过结合临床(CDMS)和MRI(新病变)状态来评估CDMS。此外,一些重要的方面只被部分地探索过。这些包括年龄和CIS地形对标准表现的影响,以及治疗开始对发生CDMS的风险的影响。最后,2017年修订版预测残疾累积的能力尚未得到调查。近日,有研究人员比较了2017年修订的McDonald标准和2010年修订的McDonald标准在诊断多发性硬化症(MS)临床孤立综合征(CIS)患者和预测预后方面的表现。
对来自欧洲9个中心的785例脑梗死患者在发病5个月后进行脑脊液检查、脑和脊髓磁共振检查,并对发病15个月内的≤进行随访。还收集了第二次临床发作的日期和达到扩展残疾状态评分(≥)3.0时的日期(如果发生的话)。2017年和2010年McDonald空间传播标准(DIS)、时间传播标准(DIT)(包括寡克隆条带评估)和DIS+DIT预测第二次临床发作(临床明确[CD])的执行情况MS)和EDSS≥3.0进行随访评估。对不同标准的多发性硬化症的诊断时间也进行了估计。
- 随访时(中位数为69.1个月),406/785名CIS患者发展为CDMS。
- 在36个月时,2017年DIS+DIT标准具有较高的敏感性(0.83比0.66)、较低的特异性(0.39比0.60)和相近的曲线下面积值(0.61比0.63)。
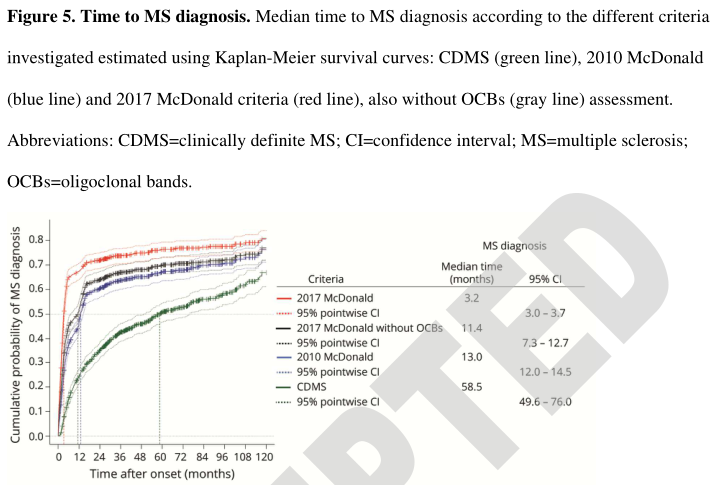
- 与2010年或CDMS标准相比,2017年MS诊断的中位时间更短(2017年修订=3.2;2010年修订=13.0;CDMS=58.5个月)。
- 这两套标准类似地预测了EDSS≥3.0的里程碑。
- 在≥45岁的患者中,3个脑室周围病变提高了特异性。
与2010年的McDonald标准相比,2017年的McDonald标准在预测CDMS方面显示出更高的敏感性、更低的特异性和相似的准确性,同时缩短了MS的诊断时间。这项研究提供了II类证据,表明与2010年的麦当劳标准相比,2017年的McDonald标准更准确地区分了CIS术后早期患者的CDMS。
文献来源:https://n.aan.80599.net/content/early/2021/10/28/WNL.0000000000013016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Neurol#
30
#综合征#
36
#ALD#
42
好的很,不错
63
完善输注原则,优先选择ABO和RhD同型
70
学习
56