Blood:受体骨髓固有巨噬细胞可显著影响造血干细胞移植预后!
2018-07-02 MedSci MedSci原创
中心点:受体巨噬细胞持续存在于在造血组织,并可在同基因移植后通过原位增殖进行自我定植。移植后,靶向耗竭受体CD169+巨噬细胞可破坏造血干细胞的长期骨髓植入。摘要:常驻组织巨噬细胞的不同亚群在造血干细胞壁龛稳态和红细胞生成过程中具有重要作用。近日,Blood杂志上发表一篇文章,Simranpreet Kaur等人在小鼠模型中利用髓系报告基因(Csf1r-eGFP)对骨髓和脾巨噬细胞亚集在经过致死性
受体巨噬细胞持续存在于在造血组织,并可在同基因移植后通过原位增殖进行自我定植。
移植后,靶向耗竭受体CD169+巨噬细胞可破坏造血干细胞的长期骨髓植入。
摘要:
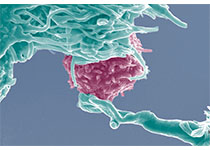
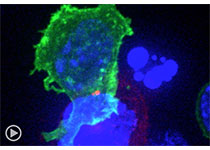
常驻组织巨噬细胞的不同亚群在造血干细胞壁龛稳态和红细胞生成过程中具有重要作用。近日,Blood杂志上发表一篇文章,Simranpreet Kaur等人在小鼠模型中利用髓系报告基因(Csf1r-eGFP)对骨髓和脾巨噬细胞亚集在经过致死性放射和自体造血干细胞移植后的持久性进行剖析。
多个受体骨髓和脾巨噬细胞亚集在自体干细胞移植后仍存活,并具有器官特异性持久动力学。受体脾脏固有巨噬细胞短期存活(5周)与髓外造血的持续时间一致。
在骨髓中,对放射耐受的受体的CD169+固有巨噬细胞和红系孤岛巨噬细胞在移植后的长时间内通过自主分裂进行自我更新增殖。移植后,受体骨髓中的CD169+固有巨噬细胞数量的峰值扩增与骨髓中表型长期重建性造血干细胞的持续性移植一致。选择性耗竭受体CD169+巨噬细胞可著着影响表型长期重建性造血干细胞移植,进而破坏重建造血。
总而言之,受体骨髓固有巨噬细胞对最佳造血干细胞移植预后至关重要,或许是进一步开发移植前调节治疗和/或耐药方法的重要考虑因素。
原始出处:
Simranpreet Kaur,et al. Self-repopulating recipient bone marrow resident macrophages promote long-term hematopoietic stem cell engraftment. Blood 2018 :blood-2018-01-829663; doi: https://doi.org/10.1182/blood-2018-01-829663
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#细胞移植#
34
#造血干细胞#
24
#造血#
31
谢谢分享学习
75
了解一下.谢谢分享!
69
学习
69
学习了.获益匪浅.感谢分享.非常不错
78