EMERG INFECT DIS:抗生素耐药性增加不利于肾盂肾炎治疗
2016-09-17 MedSci MedSci原创
近年来由于抗生素耐药性的加重导致患者患病和死亡率增加已经引起了公众关注。加州大学洛杉矶分校的研究人员进行的研究显示,抗生素耐药性的出现导致常见的肾盂肾炎更加难以治疗。 肾盂肾炎通常由大肠杆菌引起,开始表现为尿路感染,之后患者出现发热、背部疼痛和呕吐。约一半的患者需要住院治疗。如果没有有效的抗生素治疗,患者可进一步恶化为败血症和死亡。 加州大学洛杉矶分校的研究基于全国十大医院急诊中心的相关数据发现,
近年来由于抗生素耐药性的加重导致患者患病率和死亡率增加已经引起了公众关注。加州大学洛杉矶分校的研究人员进行的研究显示,抗生素耐药性的出现导致常见的肾盂肾炎更加难以治疗。
肾盂肾炎通常由大肠杆菌引起,开始表现为尿路感染,之后患者出现发热、背部疼痛和呕吐。约一半的患者需要住院治疗。如果没有有效的抗生素治疗,患者可进一步恶化为败血症和死亡。
加州大学洛杉矶分校的研究基于全国十大医院急诊中心的相关数据发现,约12%的肾盂肾炎患者对抗感染的标准用药——氟喹诺酮类抗生素(环丙沙星为常用药物)出现了耐药性,而十年前出现该药耐药性的患者仅占4%。在一些城市,具有特定风险因素(如经常国际旅行或近期住院治疗或接受抗生素治疗)的患者出现氟喹诺酮类耐药的比率超过20%。研究结果发表在Emerging Infectious Diseases。
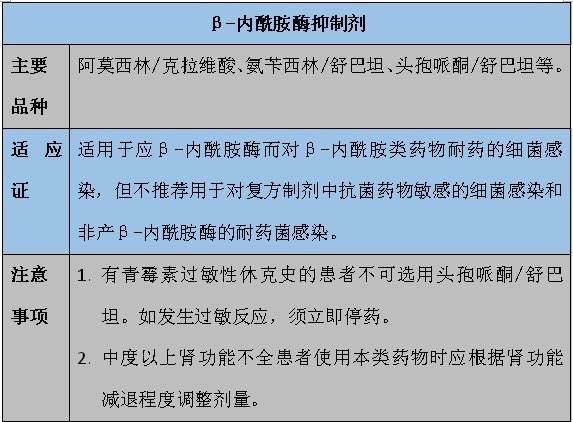
ESBL即超广谱β-内酰胺酶,是一类能水解青霉素类、头孢菌素类以及单环类抗生素的β-内酰胺酶,其活性能被某些β-内酰胺酶抑制剂抑制。能产生ESBL的细菌即为ESBL(+)菌,可对上述多种抗生素产生耐药。该酶在1979年首次被发现,通常出现在发展中国家。目前,治疗ESBL(+)菌的治疗方案只有少数静脉用抗生素治疗,而没有持续有效的口服抗生素治疗方案。加州大学洛杉矶分校的David Talan博士指出,这一新的细菌耐药菌株的出现,使抗生素治疗方案更为复杂。
这项研究包括453名于2013年7月2014年12月在全国十大医院的急诊中心诊断出患有肾盂肾炎的患者。研究人员指出,依据急诊中心方位和患者风险因素的不同,ESBL(+)菌感染的比率范围为0%-20%不等。
在感染ESBL(+)大肠杆菌的患者中,约有1/3的患者没有抗生素耐药史等风险因素,表明该菌株在美国的流行性——即便是健康的人也面临感染风险。
Talan和同事建议研发新药物,建立新的抗生素联合使用治疗标准。 他们还建议医生应密切关注当地抗生素耐药性及发生频率并及时进行尿培养或血培养确定特定的菌株。
原始出处:
[1]Increase in antibiotic-resistant bacteria hinders treatment of kidney infections.Sciencedaily.Sept.16.2016
[2]David A. Talan, Sukhjit S. Takhar,et al. Fluoroquinolone-Resistant and Extended-Spectrum β-Lactamase–ProducingEscherichia coliInfections in Patients with Pyelonephritis, United States1.Emerging Infectious Diseases.Sept.2016
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Dis#
50
总结的很好!
110
分享一下!
124
好文章,长见识
109
学习了,很受益,谢谢分享,继续关注中!
116
#抗生素耐药#
40
#肾炎#
28
#抗生素耐药性#
37