CGH: 粪便钙卫蛋白浓度在评估溃疡性结肠炎患者治疗结果中的准确性评估
2021-10-26 MedSci原创 MedSci原创
炎症的组织学特征(组织学炎症)与溃疡性结肠炎 (UC) 患者的临床复发有关。粪便钙卫蛋白 (FC) 的浓度可用于识别粘膜炎症患者。
在过去的十年中,炎症性肠病的治疗靶点发生了深刻的变化。现在,治疗成功取决于症状控制和肠粘膜愈合情况。在溃疡性结肠炎 (UC) 中,越来越多的证据表明组织学愈合与改善的结果相关,包括降低临床复发、手术和肠道纤维化的风险。粪便钙卫蛋白(FC)对UC内镜炎症的诊断准确性相对较高。一些研究表明FC值与组织学疾病活动度之间存在相关性。本项研究旨在评估FC浓度在识别组织学炎症患者方面的准确性,并开发一个模型来预测UC的治疗结果。

研究人员对接受美沙拉嗪治疗的轻度至中度UC患者的数据进行了回顾性分析。通过病历系统获得了所有患者第8周(n=639)和第52周(n=373)的临床、内窥镜和组织学数据。在第8周和第52周,使用受试者操作特征曲线下的面积来确定 FC 在识别具有不同治疗结果(临床缓解、内窥镜愈合、深度缓解或组织学缓解)的患者方面的准确性和最佳临界值。最后进行多变量逻辑回归分析以确定与这些结果相关的因素。
研究结果显示:达到临床缓解、内镜愈合、深度缓解或组织学缓解的患者的FC 浓度中位数较低。FC 浓度可以预测内窥镜愈合或组织学缓解,其接受者操作特征曲线下面积在第8周分别为0.77和0.76,在第52周分别为0.79和0.80。用于识别组织学缓解患者的最佳FC截止浓度是第8周的75 μg/g和第52周的 99 μg/g。在内窥镜评分为 0 的亚群中,组织学缓解患者的中位 FC 浓度更低。
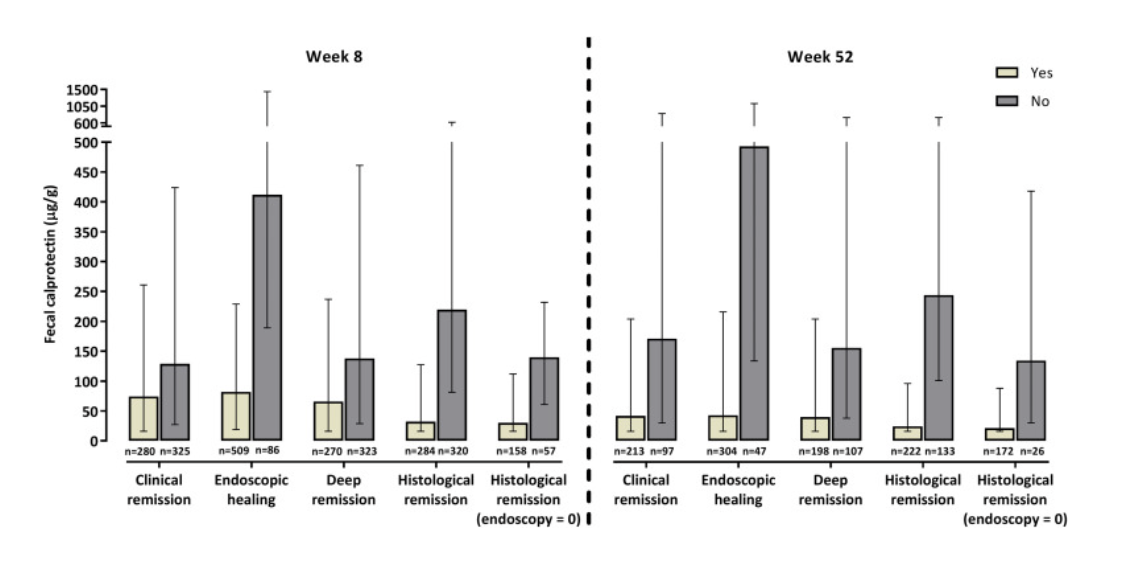
本项研究证实即使在UC完全内窥镜愈合的患者中,FC浓度也可用于区分持续微观炎症的患者和组织学缓解的患者。FC的最佳临界浓度在75到100μg/g之间。
原始出处:
Toer W. Stevens. Et al. Diagnostic Accuracy of Fecal Calprotectin Concentration in Evaluating Therapeutic Outcomes of Patients With Ulcerative Colitis. Clin Gastr H.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#溃疡性#
34
#准确性#
47
#CGH#
35
#粪便#
41
#治疗结果#
44
#浓度#
40