Lancet Oncol:每周用药的剂量密集性化疗在卵巢癌中的疗效和安全性
2022-06-13 MedSci原创 MedSci原创
与标准的3周化疗方案相比,每周给药的密集化疗方案并未改善上皮性卵巢癌患者的总体或无进展生存期
上皮性卵巢癌的标准一线化疗是卡铂联合紫杉醇(每3周给药一次)。JGOG 3016试验报道,每周予以一次紫杉醇+每三周予以一次卡铂可显著提高上皮性卵巢癌患者的无进展生存期和总生存期。但是,在另外一项试验(ICON8)中未观察到无进展生存期方面的获益。
本文报道了ICON8试验最终的总生存预后和最新的无进展生存分析结果。
ICON8试验是一项开放标签、随机、对照的3期研究,从多个国家的117家医院招募了年满18岁的新确诊的IC-IV期上皮性卵巢癌、原发性腹膜癌或输卵管癌(随后统称为卵巢癌)患者。患者被随机(1:1:1)分成三组:一组(对照组),紫杉醇(1次/3周)+卡铂(1次/3周);二组,卡铂(1次/3周)+紫杉醇(1次/周);三组,卡铂(1次/周)+紫杉醇(1次/周),每组各治疗6个21天疗程。主要终点是无进展生存期和总生存期。
2011年6月6日-2014年11月28日,共有1566位患者被随机分至一组(n=522)、二组(n=523)或三组(n=521)。中位年龄是62岁,1073位(69%)患者是高级别浆液性癌,1119位(71%)为IIIC-IV期,745位(48%)是在初次手术后入组。
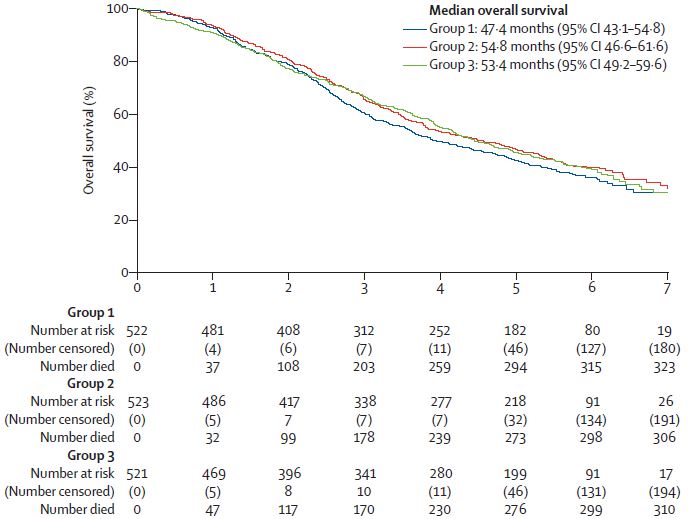
各组患者的总生存率
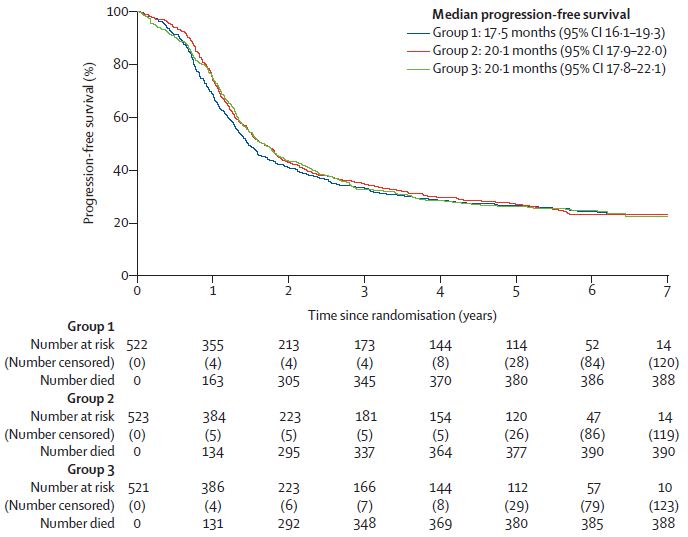
截止2020年3月31日,中位随访了69个月,与一组相比,二组和三组的总生存期均无明显差异:一组、二组和三组的中位总生存期分别是47.4个月、54.8个月和53.4个月(二组 vs 一组:HR 0.87;三组 vs 一组:HR 0.91)。在任何一项比较中也均未观察到无进展生存期方面的显著差异,一组、二组和三组的平均无进展生存期分别是23.9个月、25.3个月和24.8个月。
各组患者的无进展生存率
最常见的3-4级不良反应有中性粒细胞计数减少(一组 vs 二组 vs 三组:15% vs 36% vs 30%)、白细胞计数减少(4% vs 16% vs 14%)和贫血(5% vs 13% vs 5%)。未报道新的严重不良事件。报道了7例治疗相关死亡(2例 vs 4例 vs 1例)。
综上,该研究结果显示,与标准的3周化疗方案相比,每周给药的密集化疗方案并未改善上皮性卵巢癌患者的总体或无进展生存期,因此,不应该将其用作这类患者的一线治疗方案。
原始出处:
Andrew R Clamp, et al. Weekly dose-dense chemotherapy in first-line epithelial ovarian, fallopian tube, or primary peritoneal cancer treatment (ICON8): overall survival results from an open-label, randomised, controlled, phase 3 trial. Lancet Oncol. June 08, 2022. https://doi.org/10.1016/S1470-2045(22)00283-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#疗效和安全性#
64
#Lancet#
83
#Oncol#
47
认真学习了
47
lancet上果然牛,感谢梅斯更新及时
42