NEJM:帕博利珠单抗治疗持续性、复发性或转移性宫颈癌(KEYNOTE-826研究)
2021-09-21 MedSci原创 MedSci原创
帕博利珠单抗对化疗期间进展的程序性死亡配体 1 (PD-L1) 阳性转移性或不可切除的宫颈癌有效。我们评估了在有或没有贝伐单抗的化疗中加入派姆单抗的相对益处。
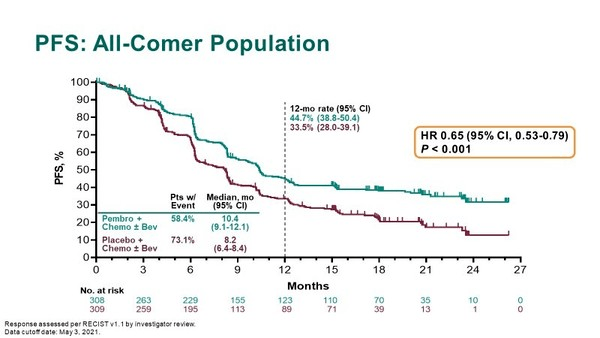
帕博利珠单抗对化疗期间进展的程序性死亡配体 1 (PD-L1) 阳性转移性或不可切除的宫颈癌有效。我们评估了在有或没有贝伐单抗的化疗中加入派姆单抗的相对益处。 在一项双盲 3 期试验中,我们以 1:1 的比例随机分配患有持续性、复发性或转移性宫颈癌的患者的一线治疗,他们没有接受过系统化疗,并且不再适合于治愈性治疗。对照组接受含铂化疗方案(紫杉醇联合顺铂或卡铂)±贝伐珠单抗,研究组的方案为帕博利珠单抗+含铂化疗±贝伐珠单抗。是否加用贝伐珠单抗由研究人员决定。每 3 周接受帕博利珠单抗(200 mg)或安慰剂治疗,最多 35 个周期加铂类药物化疗,以及根据研究者的判断加入贝伐单抗。主要终点是无进展生存期(PFS)和总生存期(OS),分别在 PD-L1 联合阳性评分为 1 或更高的患者、意向治疗人群和 PD-L1 检测10 分或以上的阳性患者。综合阳性评分定义为 PD-L1 染色细胞数除以存活肿瘤细胞总数,再乘以 100。所有结果均来自方案指定的第一次中期分析。次要终点包括客观缓解率(ORR)、缓解持续时间(DOR)和安全性。 研究结果显示: 研究组的OS相比对照组提高33%,中位OS分别为
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#复发性#
0
#持续性#
46
#转移性宫颈癌#
39
#KEYNOTE#
47
#帕博利珠#
36
#转移性#
28
#宫颈#
35