Cell Rep:新发现!巨噬细胞和神经“肝胆相照”,一同助力骨骼修复
2020-06-23 竹子 转化医学网
导言:免疫细胞在骨骼修复中显然很重要,但美国一项新研究发现有个重要角色可参与了修复过程,那就是巨噬细胞(白细胞)。它会跟神经纤维进行“对话”,配合交代敌人的来袭,促使骨头愈合。
导言:免疫细胞在骨骼修复中显然很重要,但美国一项新研究发现有个重要角色可参与了修复过程,那就是巨噬细胞(白细胞)。它会跟神经纤维进行“对话”,配合交代敌人的来袭,促使骨头愈合。
近日,美国霍普金斯大学医学院发现,巨噬细胞通过炎症提醒免疫系统对外来入侵者免疫,可以使受伤的骨骼的神经再生。该研究发表在《细胞报告》上。

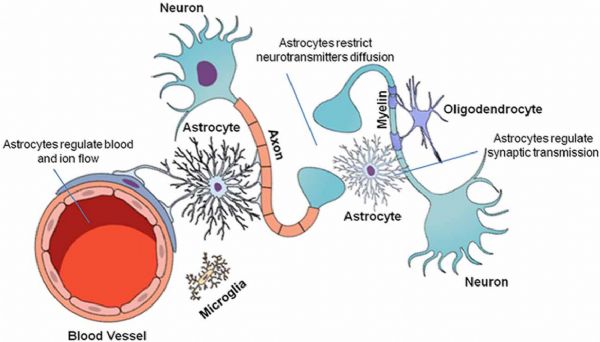
2019年12月,约翰霍普金斯大学医学院的一个研究人员团队在小鼠中证明,修复骨折需要在整个受伤区域产生、生长和扩散神经细胞或神经元。他们表明,这部分依赖于一种称为神经生长因子(NGF)的蛋白质。现在,研究人员已经更深入地研究了这个过程,以便更好地了解神经和免疫系统如何与NGF协同工作,从而使骨骼修复过程中的神经再生。
2020年5月26日,《细胞报告》杂志上发表的一项新研究中,研究人员再次在小鼠中发现,原肌球蛋白受体激酶A(TrkA)和NGF两种蛋白结合在一起,竟可以刺激神经支配(供应的神经),然后在受伤的部位再刺激新骨生长。令人惊讶的是,在这一过程中,最重要的NGF竟是巨噬细胞(即白细胞)在第一时间内发送急报给免疫系统的。巨噬细胞通过炎症提醒免疫系统,让“守卫军”们对外来入侵者免疫,然后吞噬攻击者的残骸,赶尽杀绝。
当骨头受伤时,NGF会大量释放。这会激活感觉神经,使其生长到受伤的组织中。这些感觉神经扮演着多种角色,一边作为哨兵,吹响身体疼痛的哨声,提醒骨骼的断裂;一边作为协调员,调节骨骼的愈合。
为了确定修复骨骼的机制,研究人员从每只小鼠身上取出了同一小块头骨。通过操纵不同小鼠中NGF-TrkA信号通路的各个步骤,研究小组发现:(1)NGF的释放与神经支配的开始是一致的;(2)骨损伤会刺激NGF的产生增加,(3)损伤部位的炎症会促使巨噬细胞产生NGF(由炎症过程中释放的化学信号吸引),(4)NGF的增加会引起受伤的组织中新神经的形成,(5)破坏NGF的产生会减少神经支配并损害颅骨再生(6)巨噬细胞产生的NGF是修复骨所需的神经营养物质。
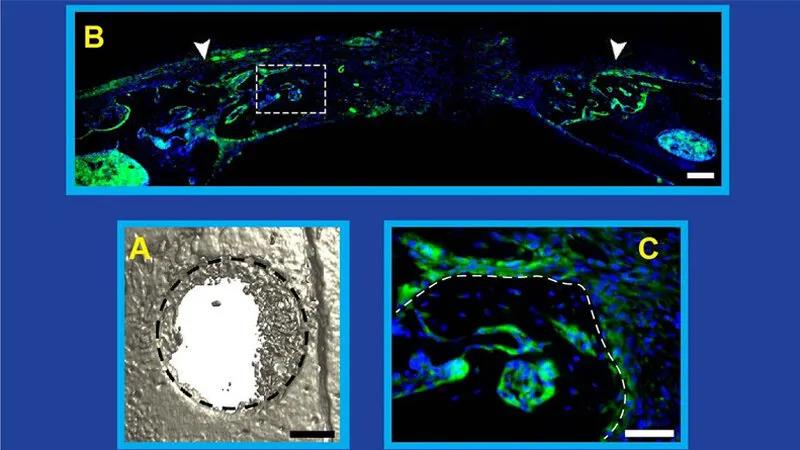
A)电脑断层扫描图像显示受伤14天后小鼠颅骨中的骨骼再生长(黑色虚线是去除的骨骼的原始部分);(B)骨修复图像(去除的原始部分在白色箭头之间)显示NGF的表达(绿色);(C)B中用虚线白框表示的部分的高放大倍率图像(C中的白虚线是愈合骨的边缘)。
研究人员表示,现在知道神经生长和骨骼修复是相互联系的过程。知道这一点,他们也许能够找到方法来最大化人的先天治愈能力。开发改善骨骼愈合的新方法将使许多人受益,尤其是老年人,毕竟摔一跤可比突发心脏病去见阎王爷的几率高。
原始出处:
Carolyn A. Meyers, Seungyong Lee, Takashi Sono, et.al. A Neurotrophic Mechanism Directs Sensory Nerve Transit in Cranial Bone. Cell Reporst VOLUME 31, ISSUE 8, 107696, MAY 26, 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cell#
33
#CEL#
0
#骨骼修复#
38
#新发现#
28