The Oncologist:Palbociclib联合内分泌治疗HR+/HER2-转移性乳腺癌的安全性分析:来自PALOMA系列5年随访综合分析更新
2021-05-15 yd2015 MedSci原创
通过5年的长期综合分析,证实Palbociclib联合内分泌治疗HR+/HER2-转移性乳腺癌是一种安全的治疗方式。
Palbociclib是一种细胞周期蛋白依赖性激酶(CDK)4/6抑制剂,与内分泌(ET)联合治疗批准用于治疗激素受体阳性(HR)/人表皮生长因子受体2阴性(HER2−)晚期乳腺癌(ABC)患者。在PALOMA系列(PALOMA-1,PALOMA-2和PALOMA-3)临床研究中,Palbociclib联合来曲唑或氟维司群较单药来曲唑或氟维司群改善HR+/HER2-转移性乳腺癌患者的无进展生存期(PFS)。虽然中生存期(OS)没有获得统计学差异,但是数值上Palbociclib联合来曲唑或氟维司群获得较长的OS。除了关注患者获得生存外,还有关注治疗相关不良事件以及生活质量。因为在真实世界中,CDK4/6 抑制剂可增加间质性肺炎和静脉血栓形成,而后者可导致更差的PFS和 OS。近期,The Oncologist杂志发表了Palbociclib治疗安全性的数据更新(基于PALOMA系列研究)。
文章更新了PALOMA系列研究中综合分析Palbociclib联合治疗5年随访安全性。数据截止时间:PALOMA-1:2017年12月21日;PALOMA-2:2017年5月31日;PALOMA-3:2018年4月13日。研究数据表明,Palbociclib联合内分泌每年治疗人次为1,421.6(n=872),而内分泌单药为528.4 (n = 471)。Palbociclib联合内分泌组中,36%患者治疗超过24个月,22.4%患者超过36个月,1.7%患者治疗超过48个月,0.7%患者治疗超过60个月,大部分患者是来自PALOMA-2试验。内分泌单药组中,20.2%患者治疗超过24个月,10.2%患者超过36个月,0.8%患者治疗超过48个月,0.4%患者治疗超过60个月。联合组中中位治疗持续时间为14.8个月 (范围: 0–84.4) ,而内分泌单药组为2.9个月 (范围: 0–74.7) 。
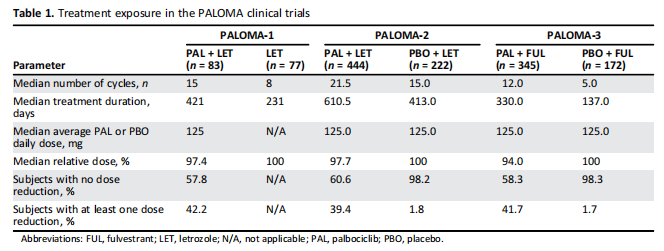
治疗持续时间对比
Palbociclib联合内分泌组发生任何级别粒细胞减少和感染分别为82.1% 和59.2%, 而内分泌单药组分别为5.1% 和 39.5%。3/4级感染的危险比为1.6(p=0.0995),3/4级病毒性感染危险比为1.8 (p = .4358) ,感染的危险比为1.4 (p = .0001) ,中性粒细胞减少危险比为30.8 (p < .0001)。Palbociclib联合内分泌组发生发热性粒细胞减少比例为1.4%。两组任何级别的血液性不良事件在治疗的第一年达到顶峰,在随后的5年治疗中较平稳。Palbociclib联合内分泌组发生间质性肺炎有13例患者,而内分泌单药治疗中有3例患者。

内分泌治疗不良事件

联合或单药治疗相关不良事件
综上,通过5年的长期综合分析,证实Palbociclib联合内分泌治疗HR+/HER2-转移性乳腺癌是一种安全的治疗方式。
原始出处:
Richard S Finn , Hope S Rugo , Karen A Gelmon,et al. Long-Term Pooled Safety Analysis of Palbociclib in Combination with Endocrine Therapy for Hormone Receptor-Positive/Human Epidermal Growth Factor Receptor 2-Negative Advanced Breast Cancer: Updated Analysis with up to 5 Years of Follow-Up. Oncologist. 2021 May;26(5):e749-e755.doi: 10.1002/onco.13684.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#Oncol#
30
#HER2-#
29
#分泌#
32
#5年随访#
58
学习学习一下
70
#palbociclib#
34
#转移性#
23
#GIST#
24
激素阳性的乳腺癌,采用CDK4/6联合内分泌治疗值得期待,希望价格患者可以承受
56
谢谢梅斯分享这么多精彩信息
44