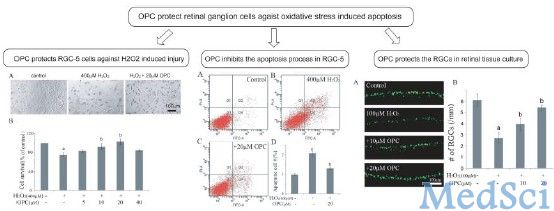
在垂体肿瘤压迫视神经交叉的管理中,通过光学相干断层扫描测量视网膜神经节细胞层厚度可为前视觉通路病变提供客观和可靠的评估,以补充视野检查。我们展示3种不同的神经节细胞层变薄模式——交界(图1A-D)、双鼻侧(图1B和E)和同侧(图1C和F)——并说明这些模式如何对应于垂体腺瘤压迫视交叉的位置,前部(图2A)、中央(图2B)或后部(图2C)。考虑神经节细胞层变薄的模式,结合视野检查,有助于前视觉通路病变部位的预测。
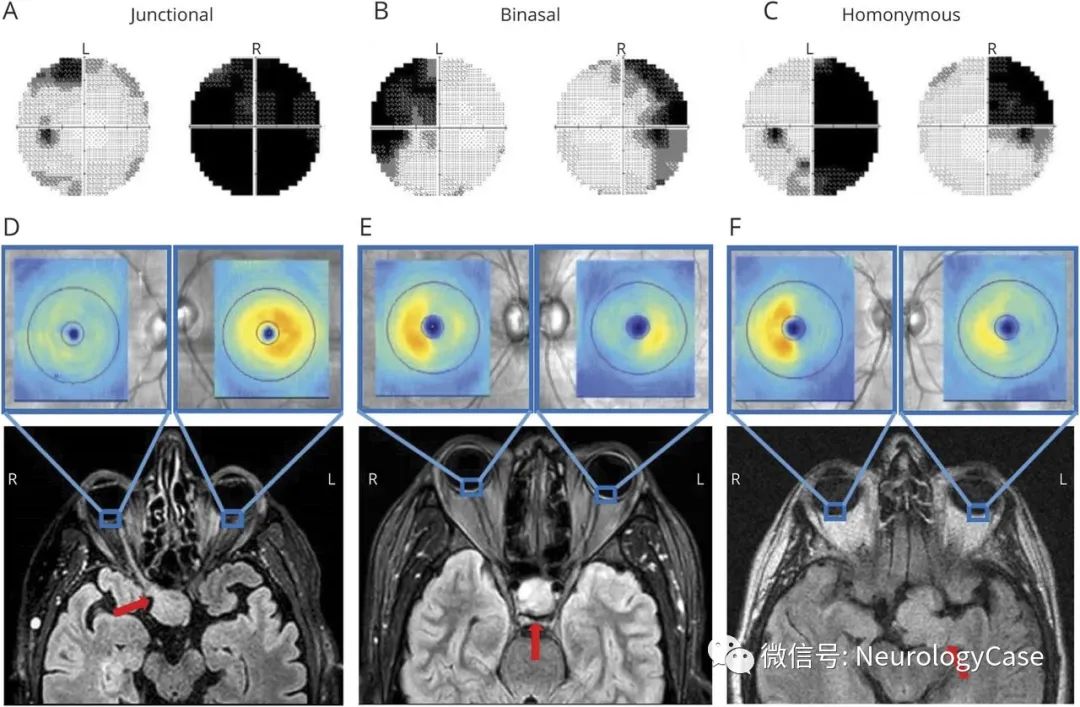
(图1:T2WI[D]上可见垂体腺瘤[红箭]压迫前部视交叉,对应于同侧眼的弥漫性视野丧失[暗区],对侧眼上颞侧交界性暗点[A]以及光学相干断层扫描[D]上同侧眼弥漫性神经节细胞变薄[蓝区]和对侧眼下鼻侧变薄;中央压迫对应于双颞侧偏盲[B]和双鼻侧神经节细胞变薄[E];后部压迫对应于[不一致的]对侧同向偏盲[C]以及同侧眼颞侧神经节细胞变薄和对侧眼鼻侧变薄[F])
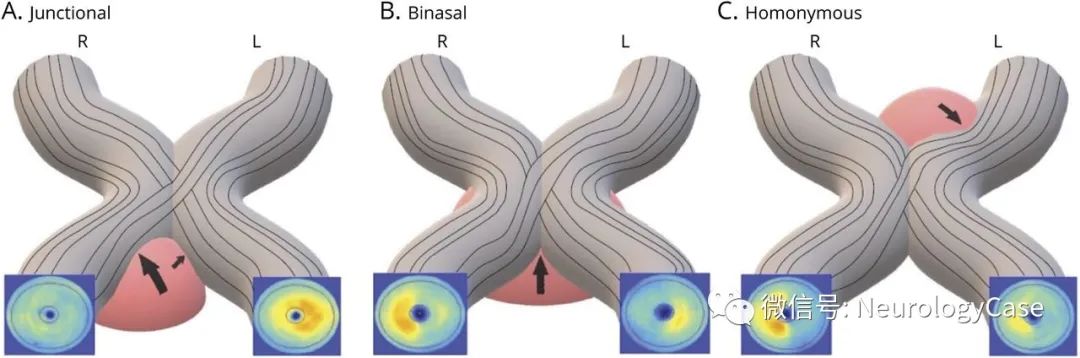
(图2:A:垂体腺瘤[粉红色]累及右侧视神经和左侧下内侧视神经[黑箭]压迫前部视交叉[灰色];B:垂体腺瘤压迫中央视交叉;C:垂体腺瘤累及左侧视束压迫后部视交叉)
[参考文献]
Miller GD, Vuong LN, Hedges TR 3rd. Teaching NeuroImage: Ganglion Cell Patterns Localize Anterior Visual Pathway Lesions. Neurology. 2021 Oct 19;97(16):e1637-e1638.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#神经节细胞#
35
#Neurol#
45
#视觉通路#
33
#视觉#
47