微小转移灶的自发消退:原发性肿瘤分泌物的关键作用
2020-03-17 医学论坛网 医学论坛网
手术切除原发肿瘤是癌症治疗的基石,肿瘤摘除术后转移灶消失的原理,是业界感性去的话题之一。有学者认为,存在于原发性肿瘤的抑制性信号对这一过程起着重要作用。
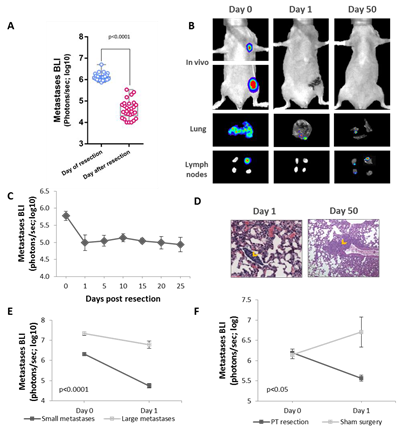
研究者首次提出了切除原发肿瘤后转移灶自发消退的动物模型,该模型采用了癌细胞高度敏感的荧光素酶报告基因,从而能够研究早期的微转移,结果发现微转移的发展受到PT分泌的众多因素的支持,而PT及其分泌因子的去除可诱导早期转移的消退。识别特定的潜在因素,并中和其中的四个因素,可以阻止癌症转移的进程。
使用表达高度敏感的荧光素酶MDA-MB-231HM乳腺癌细胞,监测BALB / c nu / nu小鼠自发转移发展的早期阶段。
切除PT引起最小转移灶明显消退,但较大的转移灶没有消退,并且体内补充肿瘤分泌组减少了这种消退,表明PT分泌的因子促进早期转移性生长。
相应地,癌细胞条件培养液在体外减少凋亡并增强MDA-MB-231HM粘附。为了鉴定特定的介导因子,研究者分析了MDA-MB-231HM分泌组的细胞因子阵列和蛋白质组学。
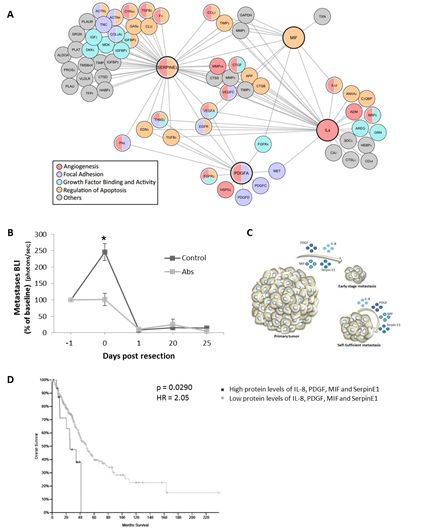
结果发现显著丰富的血管生成、生长因子结合和活性、粘着斑、金属蛋白酶调节和细胞凋亡调节过程。
在体内同时阻断这些过程的四个分泌关键介质、IL-8、PDGFaa、丝氨酸蛋白酶抑制剂E1(PAI-1)和MIF,在PT的存在下阻止了微转移的发展。
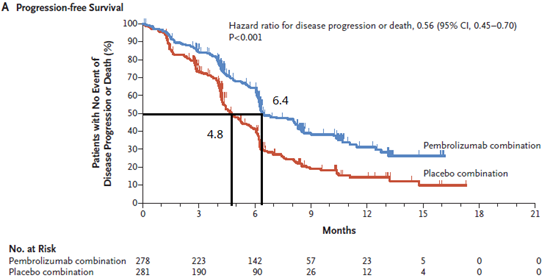
有趣的是,根据TCGA数据集,这四个因子的高蛋白水平与肺腺癌患者的不良生存率相关。
这些结果证明了PT切除后微转移的消退和潜伏期,以及PT-分泌组在促进MDA-MB-231HM异种移植早期转移阶段中的关键作用。
这些发现可能表明控制PT切除期间和之后的最小残留疾病的新方法。
为了检查原发性肿瘤切除对转移性生长的影响,将MDA-MB-231HM细胞注射到裸鼠的乳腺脂肪垫中以形成原发性肿瘤。
在这种原位模型中,肿瘤植入后2-4周,在淋巴结和肺中自发形成远处转移灶。当转移的胸部定位生物发光信号达到106个光子/秒的总通量时,切除了原发肿瘤。在肿瘤切除后的24小时内,小鼠的转移信号急剧下降,最高可达100倍。

由于已经提出了几种解释自发消退的机制,研究者首先试图区分由手术本身引起的影响(例如炎症和血管功能不全)和切除肿瘤有关的影响,原发性肿瘤的促转移性分泌因子(即生长因子、细胞因子和血管生成因子)的分布。为此,对小鼠进行假手术(保留20个原发性肿瘤)或原发性肿瘤切除。切除原发肿瘤后转移明显消退,而接受假手术的小鼠继续发生转移。
为了确定在原发肿瘤切除后其介导转移灶自发消退的因素,采用人类细胞因子阵列分析了肿瘤分泌组。分析了4种情况:(i)肿瘤细胞条件培养基(CM);(ii)非肿瘤小鼠;(iii)携带原发肿瘤的小鼠和(iv)肿瘤切除后一天的小鼠的血浆样品。鉴定了28种在癌细胞CM中高度表达的细胞因子。然后排除了5个在非肿瘤小鼠血浆和/或肿瘤切除后小鼠血浆中也很明显的因子。
这种选择方法针对已知发挥促转移或促生存作用的四个因素,因此将其清除可能会导致自发性消退:白细胞介素8(IL-8)、血小板衍生生长因子aa(PDGFaa )、丝氨酸蛋白酶抑制剂E1(也称为纤溶酶原激活物抑制剂1;PAI-1)和巨噬细胞迁移10抑制因子(MIF)。
为了补充这种“缩小”方法,使用了CM的无偏质谱蛋白质组学分析方法,并鉴定出2600种蛋白质,其中359种被基因本体论(GO)分析标注为细胞外因子,包括使用 细胞因子阵列。对359种细胞外蛋白的途径富集分析确定了参与转移关键步骤的蛋白,包括凋亡、血管生成、生长因子活性、粘着斑和金属酶调节。
假设这四个因素是推动转移性生长的因素,那么它们在体内的阻断作用将部分模拟原发肿瘤去除的作用并抑制转移。为进行对比,在肿瘤切除前的24 h早期转移阶段注射了针对IL-8、PDGFaa、丝氨酸蛋白酶抑制剂E1和MIF与IgG对照的小鼠抗人抗体混合物。
这些因子的抗体中和作用完全阻止了转移进程。可以预期,切除后第1天两组之间的转移消退没有明显差异,可能是因为完全切除了两组中的所有分泌因子。这些发现表明,这些主要的肿瘤分泌因子是早期微转移生存的关键因素,而已确立的较大转移灶可能是自给自足的。
这项研究表明,MDA-MB-231HM肿瘤分泌基因组在远处转移灶的生存和发展中起着至关重要的支持作用,并证明了原发MDA-MB-231HM肿瘤切除后的转移性退化现象。已知维持和促进转移的IL-8、MIF、SerpinE1和PDGFaa蛋白,表明它们在PT存在下的体内中和作用阻止了转移进程。根据公开的TCGA临时数据集,这四种因子的高蛋白水平与一组肺腺癌患者的不良生存率相关。因此,肿瘤分泌因子可能通过多种机制起作用,从而影响恶性细胞和/或其微环境。这些发现为确定新的预防和治疗策略提供了机会。
原文链接:
https://www.biorxiv.org/content/10.1101/2020.03.12.986992v1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#原发性#
40
#分泌#
0
#分泌物#
45
#转移灶#
48
#原发性肿瘤#
48