JAMA Pediatrics:每天看屏幕时间超过2小时,早产儿孩子更容易变傻
2021-07-16 MedSci原创 MedSci原创
研究发现,在 6 岁和 7 岁出生的极早产儿(在怀孕第 28 周之前)中,每天看屏幕时间超过两小时的儿童更有可能在整体智商、执行功能(解决问题的能力)、冲动控制和注意力方面出现缺陷
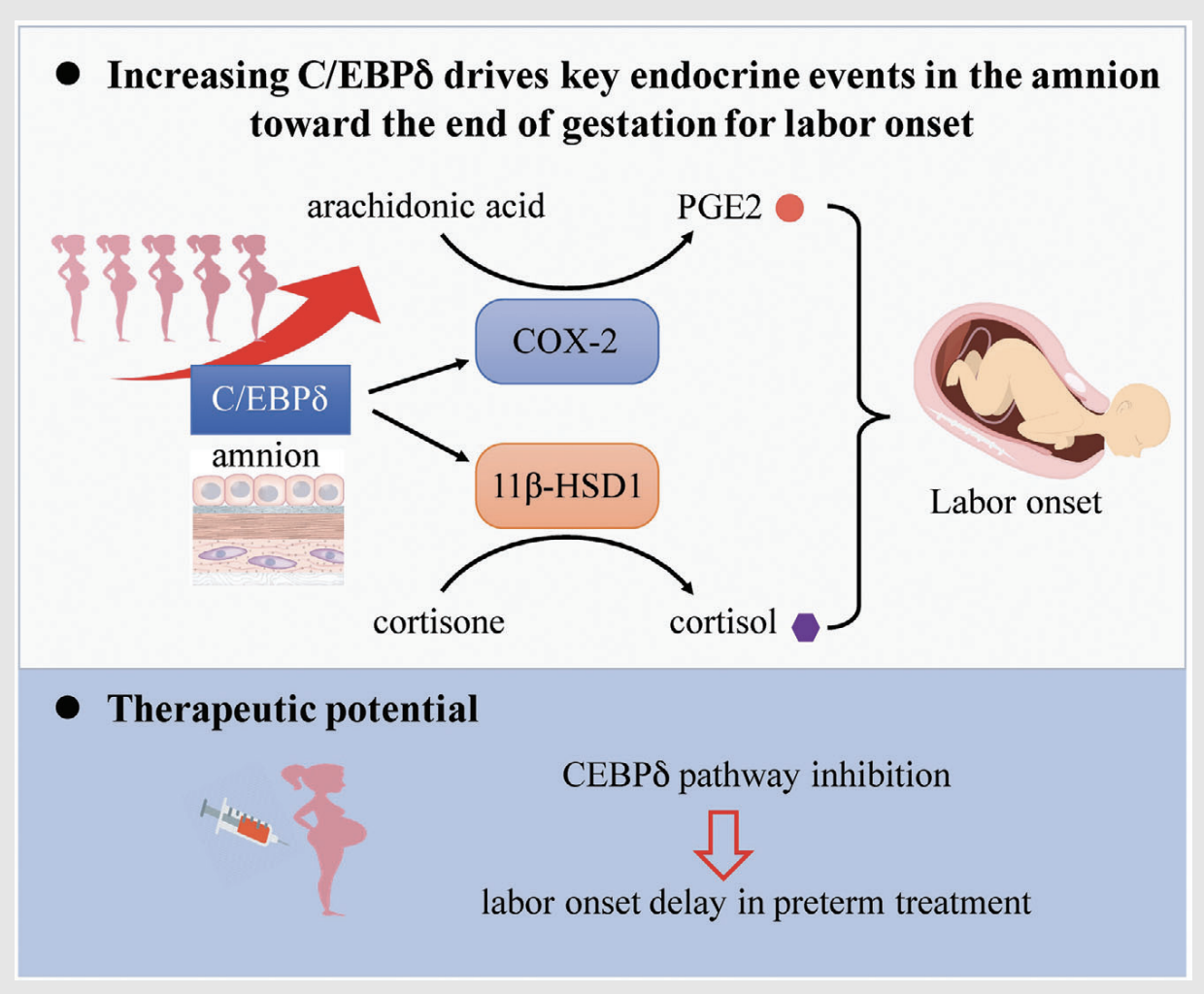
众所周知,早产和看屏幕时间增加都与发育和行为后遗症的风险增加有关。学龄前长时间看电视或卧室里的电视或电脑与极早产儿 (EPT) 的不良认知、执行功能、语言和行为结果之间的关系尚不清楚。

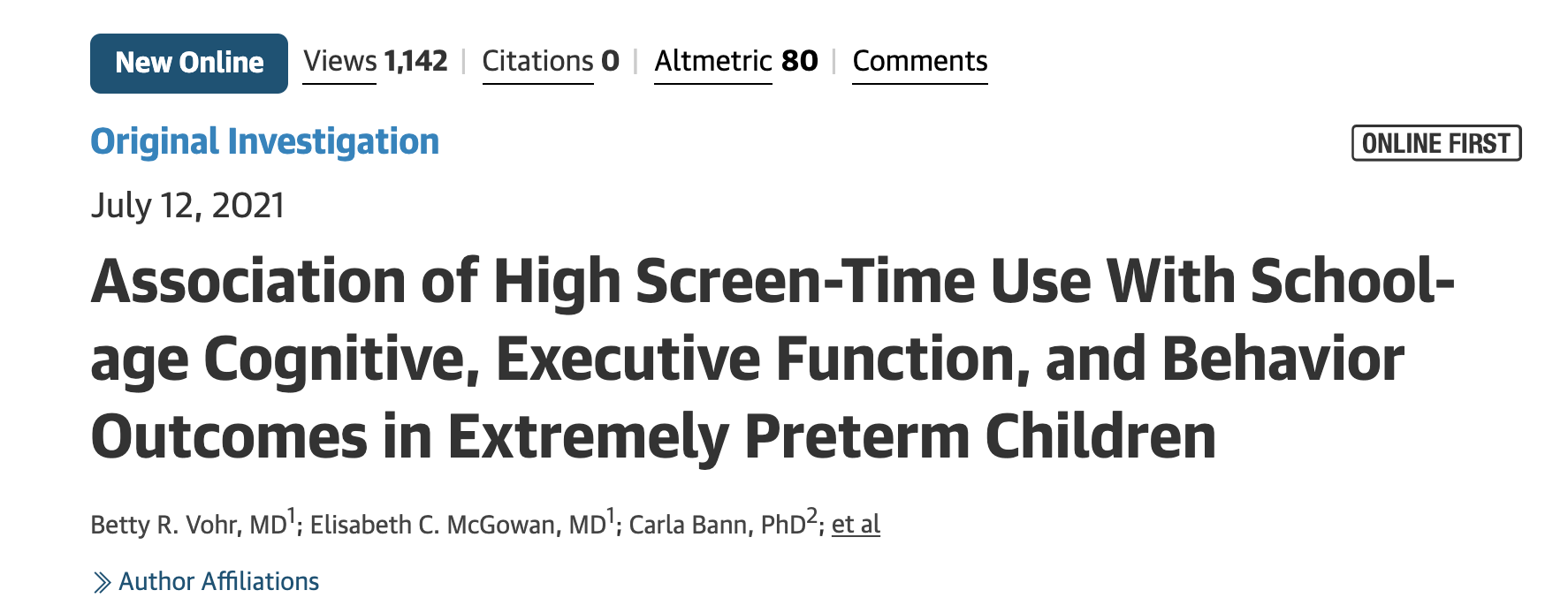
近期,一项发表在 JAMA Pediatrics的研究表明,每天 2 小时或更多的屏幕时间与极早产儿在学龄前出现认知、执行功能和行为问题的风险增加有关。研究发现,在 6 岁和 7 岁出生的极早产儿(在怀孕第 28 周之前)中,每天看屏幕时间超过两小时的儿童更有可能在整体智商、执行功能(解决问题的能力)、冲动控制和注意力方面出现缺陷。同样,卧室里有电视或电脑的人更有可能在冲动控制和注意力方面出现问题。
在当前的研究中,研究人员分析了一项对 28 周或更早出生的儿童的研究数据。研究员评估了6~7岁EPT儿童高屏幕时间与认知、语言、执行功能和行为的相关性;第二个目标是检查高屏幕时间与结构化身体活动率和体重之间的关联。
纳入分析的 414 名儿童中,男孩 227 人(55%);平均 (SD) 出生体重为 870.6 (191) g。共有 238 名儿童 (57%) 的看屏幕的时间较长,每天的屏幕时间超过两个小时,266 名 (64%) 儿童的卧室里有电视/电脑。
研究结果发现,与每天屏幕时间较少的儿童相比,屏幕时间较长的儿童在全球执行功能百分位得分上平均差近 8 分,在冲动控制(抑制)方面低约 0.8 分,在注意力不集中方面高出 3 分以上. 在卧室里有电视或电脑的孩子在抑制、多动和冲动方面的得分也较低。
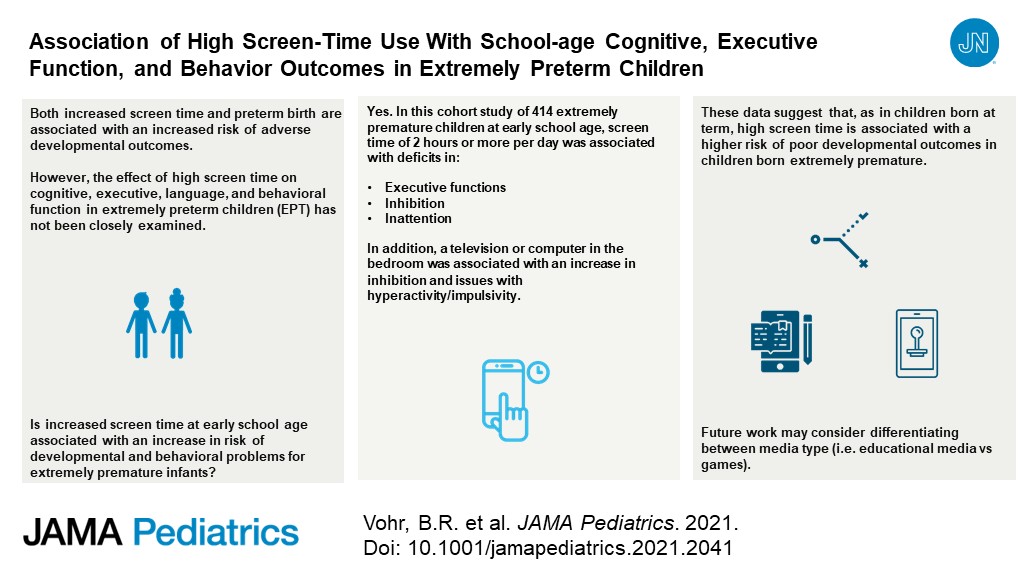
综上, 本研究的结果表明,在出生不足 28 周的儿童中,长时间的屏幕时间会导致 6 至 7 岁的不良认知、执行功能和行为结果。这些发现支持医生与极早产儿家庭讨论屏幕时间的潜在影响的必要性。
参考文献:Vohr, BE, et al. Association of high screen-time use with school-age cognitive, executive function, and behavior outcomes in extremely preterm children. JAMA Pediatrics.2021. DOI: 10.1001/jamapediatrics.2021.2041
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#Pediatric#
50
#DIA#
45
#PE#
48
可怕
71
学习一下
77
好
79
学习了
69
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
51
…
57