Clin Trans Gastroenterology:扩大肠系膜切除术在克罗恩结肠炎术后复发中的作用
2021-10-08 MedSci原创 MedSci原创
克罗恩病 (CD) 是一种慢性炎症性肠病,多达 78% 的 CD 患者需要手术干预。大约 20% 的患者在 10 年内会出现复发,需要进一步手术治疗。
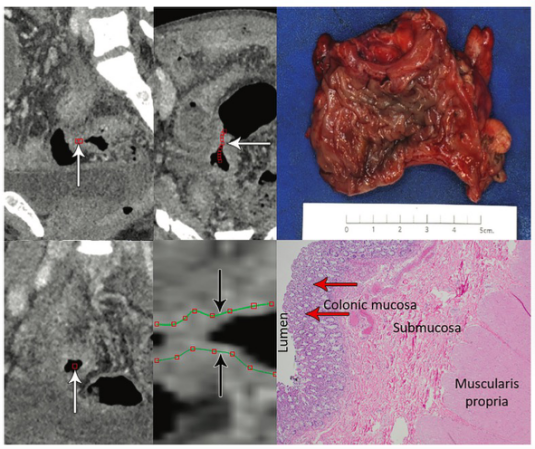
克罗恩病 (CD) 是一种慢性炎症性肠病,多达 78% 的 CD 患者需要手术干预。大约 20% 的患者在 10 年内会出现复发,需要进一步手术治疗。越来越多的证据表明肠系膜参与 CD的发生发展,肠系膜切除边缘的肠系膜淋巴管密度增加以及肠系膜淋巴结中肉芽肿的存在与术后复发率的增加有关。在 CD 和溃疡性结肠炎等良性疾病的结直肠切除手术中,保守方法(即保留肠系膜)和广泛的肠系膜切除术(类似于完全系膜切除术)均根据外科医生的自己判断进行。最近的一项研究报告称,在 CD 回结肠切除术中切除肠系膜与减少手术复发有关。本研究旨在探究接受结肠直肠手术的克罗恩结肠炎 (CC) 患者肠系膜切除术与术后结果之间的关联。
研究人员通过病历系统回顾了 2000 年 1 月至 2018 年 12 月期间接受结直肠切除术的 CD患者的临床资料。根据肠系膜切除范围将患者分为2组,广泛肠系膜切除(EME)组和限制性肠系膜切除(LME)组,然后比较两组的预后,包括术后早期发病率和手术复发率。
在纳入的 126 名患者中,LME 组有 60 名,EME 组有 66 名。除了 LME 组术中失血量增加外,两组在术后早期结果方面没有显着差异(P = 0.2)。与 LME 组相比,EME 组患者的术后无复发生存时间更长(P = 0.01)。LME 是术后手术复发的独立预测因子(HR 2.67,95%CI: 1.04-6.85,P = 0.04)。这在接受结直肠切除和吻合术的患者的亚组分析中得到了进一步证实(HR 2.83,95%CI:1.01-7.96,P = 0.048)。
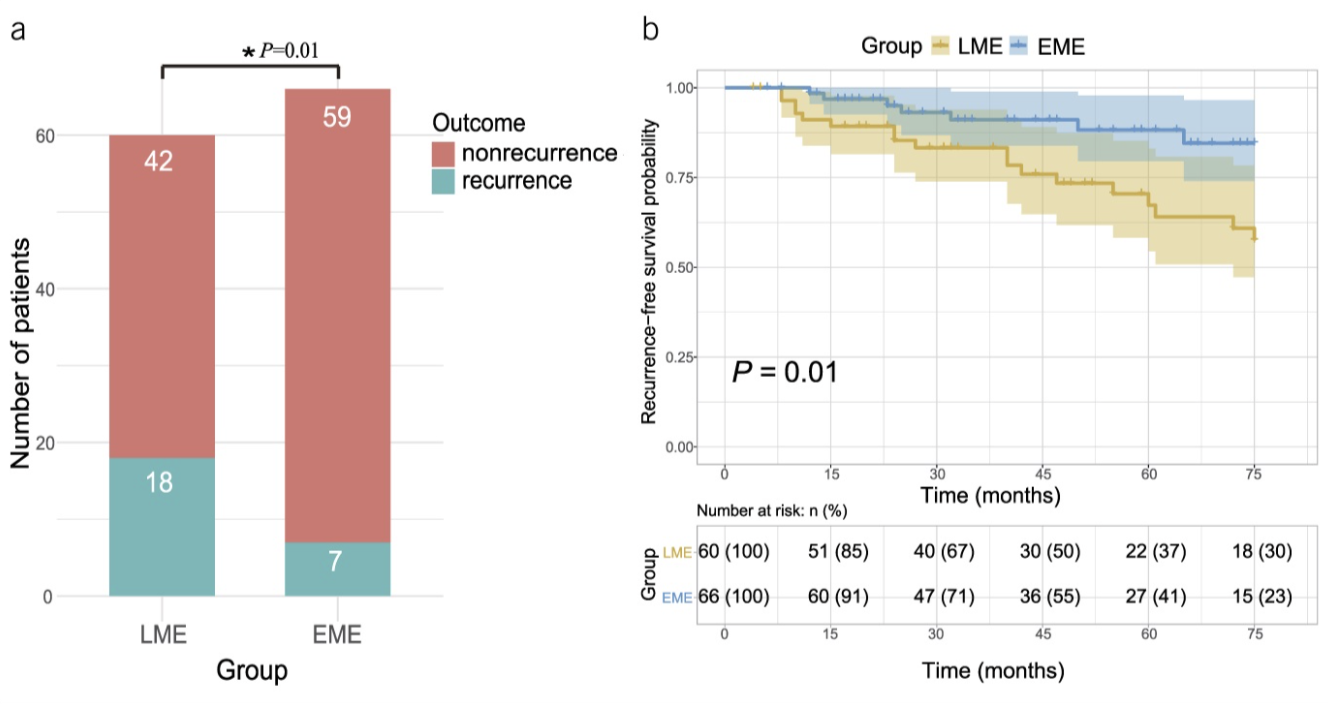
本项研究证实在接受结直肠切除手术的CD患者中,与保留肠系膜相比,扩大切除肠系膜与长期结果改善相关。
原始出处:
Zhu, Yipeng. Et al. Role of Extended Mesenteric Excision in Postoperative Recurrence of Crohn's Colitis: A Single-Center Study. Clinical and Translational Gastroenterology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#术后复发#
37
#Gastroenterol#
28
#GAS#
39
#TRA#
31
#AST#
36
#切除术#
32
#Gastroenterology#
28
#肠系膜#
38