百奥赛图与LiberoThera共同开发全人GPCR抗体药物取得里程碑式进展
2022-07-21 网络 网络
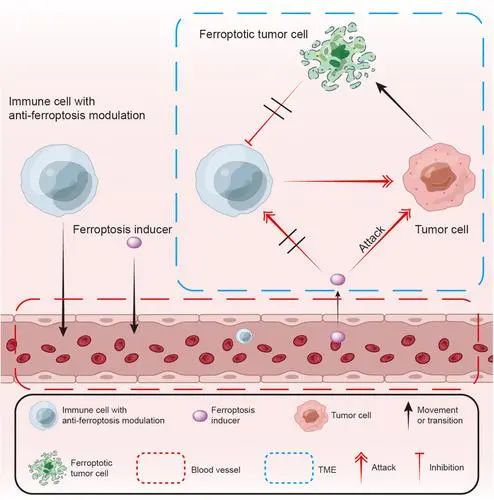
机制上,这些克隆可通过增强的ADCC效应来耗竭肿瘤微环境中的Treg,也可通过抑制其配体CCL1介导的CCR8信号通路来抑制肿瘤微环境中的Treg活性,进而达到增强抗肿瘤免疫反应的目的
2021年2月1日,百奥赛图(北京)医药科技股份有限公司(“百奥赛图”)与日本LiberoThera有限公司(“LiberoThera”)共同宣布,基于百奥赛图世界先进的全人抗体小鼠RenMab®的抗体发现平台及LiberoThera杰出的膜蛋白抗原制备技术,双方共同开展针对全人GPCR抗体开发的战略合作。自合作达成以来短短一年左右的时间里,双方就已针对首个合作靶点CCR8,筛选到体外和体内抗肿瘤活性都优秀的多个全人治疗性抗体克隆,具有成为同类最佳产品的潜质。这些克隆具有高亲和力结合人CCR8并可跨物种交叉识别,生产工艺简易等优良特性。机制上,这些克隆可通过增强的ADCC效应来耗竭肿瘤微环境中的Treg,也可通过抑制其配体CCL1介导的CCR8信号通路来抑制肿瘤微环境中的Treg活性,进而达到增强抗肿瘤免疫反应的目的。未来,双方合作还将拓展到其他GPCR靶点。
GPCR是七次跨膜蛋白,胞外区短,不同GPCR间同源性高,故而难以找到特异性强,且具有目标功能的抗体。基于百奥赛图的靶点敲除全人抗体小鼠RenMab KO、多种免疫及抗体发现技术手段和高通量体外体内筛选平台,以及LiberoThera对GPCR靶点结构的深入理解和膜抗原制备技术,GPCR抗体发现的成功率和速度都大大增加。
百奥赛图创始人、董事长兼CEO沈月雷博士表示:“很高兴在我们和LiberoThera的共同努力下,针对肿瘤免疫治疗的潜力靶点CCR8的药物研发进展顺利。这无疑证实了LiberoThera先进的抗原制备技术与我们的RenMice KO平台强强联合,可以促进多样性全人抗体的产生。结合百奥赛图的高通量的体内和体外筛选能力,可有效获得针对GPCR的有效抗体。我们期待着CCR8抗体能够早日推进至临床,也期待着与LiberoThera共同攻克更多的GPCR靶点。”
LiberoThera公司的CEO Toru Kanke博士表示,“许多GPCR是多种适应症的重要的药物靶点,但由于这类靶点的结构特殊,针对它们的抗体药物开发一直面临挑战。用LiberoThera自有的无细胞膜合成技术以及非天然氨基酸掺入方法制备的保有GPCR结构的抗原为产生针对挑战性靶点的优质抗体提供了解决方案。百奥赛图的一体化全人抗体开发平台极大地加速了对GPCR靶点研究的转化。我们很高兴地看到双方合作进展迅速,并发现了针对CCR8的同类最佳治疗性抗体。我们也期待日后与百奥赛图的合作能够快速推进至多个靶点,打开GPCR抗体研究的新局面,造福全球病患。”
关于百奥赛图GPCR抗体发现平台
GPCR (G protein-coupled receptor)蛋白是人类基因组中数目最庞大的膜蛋白。在已上市的药物中,有1/3的药物作用于GPCR蛋白。针对GPCR的抗体药物不仅可以激活或阻断GPCR信号通路,还可以通过抗体的ADCC或ADCP等效应直接靶向消灭病变细胞。然而,由于抗原制备困难、缺少高通量筛选方式等原因,GPCR抗体开发面临巨大挑战,目前发现的GPCR可成药靶点有370个,但其中只有2个已成药,大量有价值的GPCR靶点还有待于挖掘。
为提高针对GPCR的抗体发现成功率,百奥赛图现已建立起完善的GPCR抗体发现平台。通过多种GPCR抗原,如DNA抗原,来免疫靶点基因敲除的RenMiceTM鼠(RenMice KO),直接获得针对此靶点的全人抗体。这不但免去了抗体人源化的时间,也避免了抗体亲和力在人源化的过程中降低;同时,靶点敲除鼠由于解除了其对GPCR靶点的免疫耐受,所以免疫后能够产生表位更加丰富的抗体,提高后续抗体发现的成功率,也提高了发现多物种交叉识别抗体的可能性,利于后续的体内药效验证、安全性评估和临床转化。
结合自有的基于Beacon的高通量抗体筛选平台,可以快速筛选到具有高特异性和高亲和力的全人GPCR抗体。通过自建的基因编辑报告细胞系和人源化小鼠,可进行规模化的体外体内药效分析,实现GPCR抗体药物的大量、快速发现。
目前,针对GPCR靶点,百奥赛图“千鼠万抗”计划已有多个项目启动,涵盖单抗、双抗等药物形式,用于治疗肿瘤、代谢等疾病。目前,ADGRE1,C5AR1,CCR9,CXCR4, GPRC5D等15个靶点已获得结合人GPCR的抗体序列,更多靶点正在探索中。百奥赛图希望与全球合作伙伴共同推进针对GPCR及其他有价值的困难靶点的抗体药物开发,持续产出新药,造福病患。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#GPCR#
56
#里程碑#
55
#ERA#
39
#抗体药#
37
#抗体药物#
39
#PCR#
28