J Clin Oncol:杜瓦鲁单抗联合奥拉帕利治疗初治的转移性尿路上皮癌的疗效和安全性
2022-06-24 MedSci原创 MedSci原创
杜瓦鲁单抗加用奥拉帕利并不能提高未选择的转移性尿路上皮癌患者的生存预后
同源重组修复基因突变 (HRRm) 在尿路上皮癌 (UC) 中很常见,使肿瘤细胞对聚 (ADP-核糖) 聚合酶 (PARP) 抑制敏感。BAYOU研究评估了抗PD-L1抗体杜瓦鲁单抗联合奥拉帕利(PARP抑制剂)治疗转移性尿路上皮癌(mUC)的疗效和安全性。
该研究是一项多中心、随机、双盲的2期试验,招募了未治疗的铂类不适用的mUC患者,随机(1:1)分成两组,予以杜瓦鲁单抗(1500mg/4周)+奥拉帕利(300mg·2次/天,口服)或杜瓦鲁单抗+安慰剂治疗。主要终点是无进展生存期(PFS),次要终点包括总患者人群的总生存期和HRRm患者的PFS。
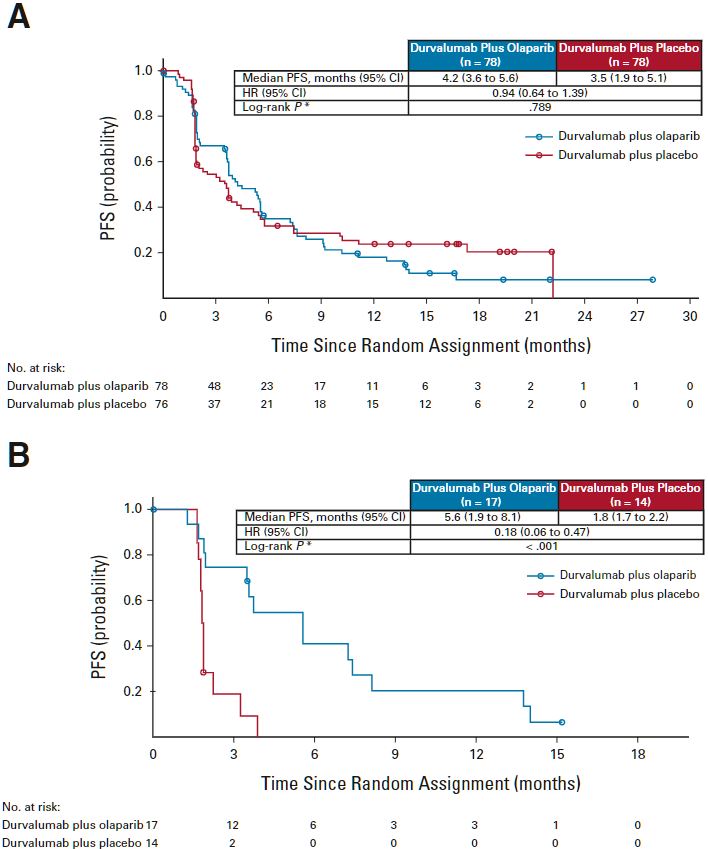
总患者和HRRm患者的PFS
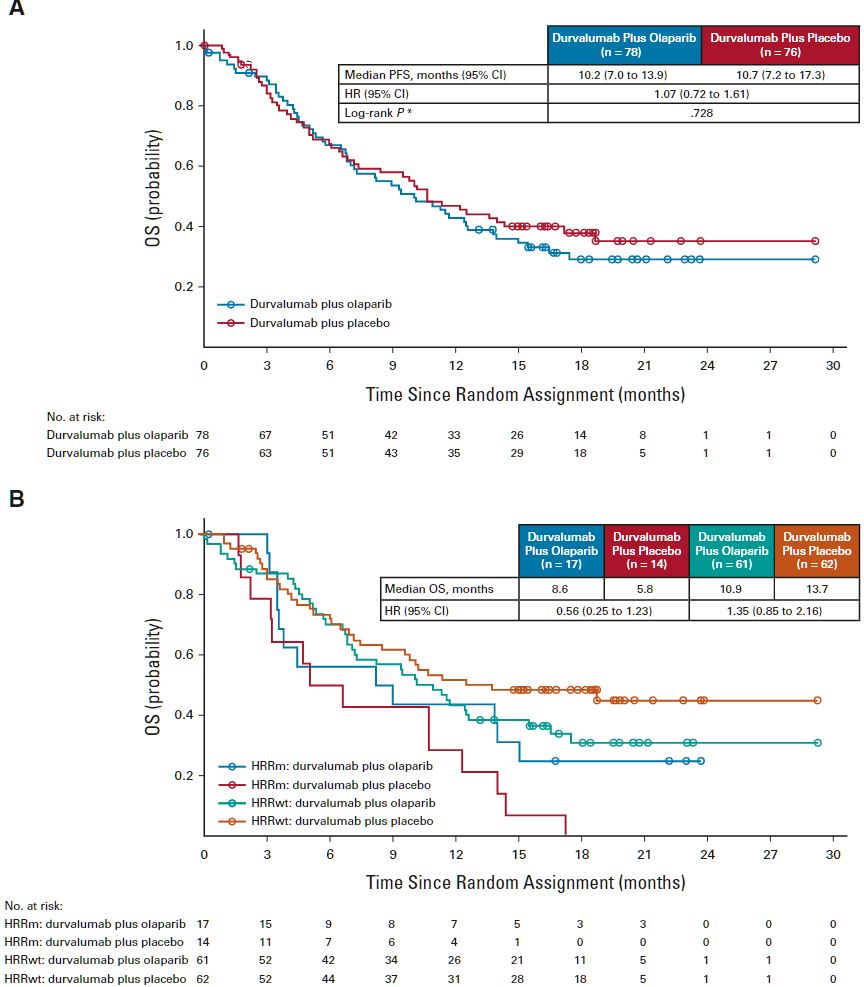
总体上,杜瓦鲁单抗+奥拉帕利组和杜瓦鲁单抗+安慰剂组的中位PFS分别是4.2个月和3.5个月(HR 0.94,p=0.789)。两组的中位总生存期分别是10.2个月和10.7个月(HR 1.07)。在20%的有HRRm的患者中,杜瓦鲁单抗+奥拉帕利组和杜瓦鲁单抗+安慰剂组的中位PFS分别是5.6个月和1.8个月(HR 0.18)。两组3/4级的治疗相关的不良事件的发生率分别是18%和9%。
总患者和HRRm患者的OS
总之,在杜瓦鲁单抗治疗的基础上,加用奥拉帕利并不能提高未选择的转移性尿路上皮癌患者的生存预后。杜瓦鲁单抗的疗效结果与其他抗PD-1/PD-L1药物报告的结果相似。但是,次要分析结果显示PARP抑制在携带同源重组修复基因突变的转移性尿路上皮癌患者中具有潜在抗肿瘤作用。
原始出处:
Jonathan E. Rosenberg, et al. Durvalumab Plus Olaparib in Previously Untreated, Platinum-Ineligible Patients With Metastatic Urothelial Carcinoma: A Multicenter, Randomized, Phase II Trial (BAYOU). Journal of Clinical Oncology. June 22, 2022. https://ascopubs.org/doi/full/10.1200/JCO.21.02829
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Oncol#
0
#疗效和安全性#
50
#转移性#
51
#转移性尿路上皮癌#
42
#上皮癌#
52