JACC:侵入性牙科手术前抗生素预防可降低术后感染性心内膜炎风险
2022-09-10 MedSci原创 MedSci原创
在高感染性心内膜炎风险的人群中,侵入性牙科手术(特别是拔牙和口腔外科手术)与随后发生感染性心内膜炎的风险相关,术前抗生素预防可降低感染性心内膜炎发生率
在侵入性牙科手术 (IDPs) 前建议使用抗生素预防 (AP),以预防高危人群感染性心内膜炎 (IE),但很少有数据支持侵入性牙科手术与感染性心内膜炎的关联或抗生素预防在感染性心内膜炎预防中的有效性。
该研究旨在调查侵入性牙科手术与感染性心内膜炎之间的关联,以及抗生素预防减少感染性心内膜炎的效果。
这是一项病例交叉分析和队列研究,研究人员对7951972位美国受试者进行了侵入性牙科手术和感染性心内膜炎以及抗生素预防疗效之间的关联分析。
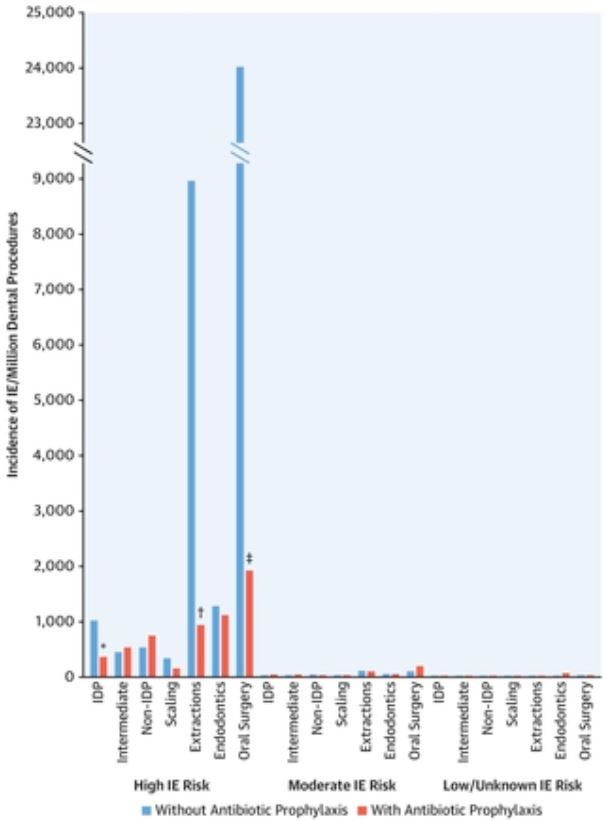
术前有无使用抗生素预防患者感染性心内膜炎的发生率
时间进程研究表明,感染性心内膜炎最有可能发生在侵入性牙科手术后的4周内。对于那些有高感染性心内膜炎风险的患者,病例交叉分析显示,感染性心内膜炎和国内流离失所者在之前4周内进行过侵入性牙科手术存在显著的时间相关性(OR 2.0,p=0.002)。这种相关性在拔牙(OR 11.08, p<0.0001)和口腔外科手术(OR 50.77,p<0.0001)时最强。
抗生素预防与侵入性牙科手术后感染性心内膜炎发生率显著降低相关(OR 0.49, p=0.01)。该队列研究证实了在感染性心内膜炎的高危人群中,感染性心内膜炎与拔牙或口腔外科手术之间的关联以及抗生素预防降低这种关联的效果(拔牙:OR 0.13,p<0.0001;口腔外科手术:OR 0.09, p=0.002)。
综上,该研究证实了在高感染性心内膜炎风险的人群中,侵入性牙科手术(特别是拔牙和口腔外科手术)与随后发生感染性心内膜炎的相关性,以及抗生素预防与这些术后感染性心内膜炎发生率降低的相关性。该研究数据支持当下的指南建议,即高感染性内膜炎风险患者在接受侵入性牙科手术前可使用抗生素预防。
原始出处:
Martin H. Thornhill, et al. Antibiotic Prophylaxis Against Infective Endocarditis Before Invasive Dental Procedures. J Am Coll Cardiol. 2022 Sep, 80 (11) 1029–1041
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#侵入性#
59
#感染性#
50
#JACC#
60
#内膜#
58
#ACC#
57
#心内膜炎#
48
#牙科#
32