Brit J Cancer:乳房X线微钙化灶与乳腺癌风险
2021-06-15 MedSci原创 MedSci原创
微钙化灶群是BC的独立危险因素,绝经前妇女的估计风险更高。在绝经后女性中,微钙化灶群与BC之间的关联与基线MD类似。
乳房X线微钙化被认为是乳腺癌 (BC) 的早期迹象。

近日,肿瘤学领域权威杂志British Journal of Cancer上发表了一篇研究文章,研究人员评估了微钙化灶群与整体和亚型特异性BC风险之间的关联。此外,研究人员分析了乳房X线检查结果上密度 (MD) 如何影响微钙化灶与BC风险之间的关联。
研究人员使用了瑞典女性的前瞻性队列 (n = 53,273),这些参与者具有关于BC危险因素和乳房X线检查照片的全面信息。研究人员分别采用计算机辅助检测系统和STRATUS方法测量了微钙化灶的总数和MD。此外,研究人员采用Cox 回归和Logistic回归进行数据分析。
微钙化灶与乳腺癌特点
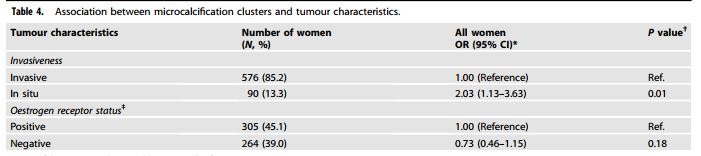
该研究中总共有676名女性被诊断为BC病例。与没有微钙化灶的女性相比,具有3个以上微钙化灶的女性风险比[HR]为2.17(95%置信区间[CI]=1.57-3.01)。绝经前妇女的估计风险更为明显(HR=2.93;95%CI=1.67-5.16)。对于绝经后妇女,微钙化灶和MD对BC风险有类似的效应。在微钙化灶和MD之间没有观察到相互作用。微钙化灶与原位乳腺癌显著相关(比值比:2.03;95%CI=1.13-3.63)。
由此可见,微钙化灶群是BC的独立危险因素,绝经前妇女的估计风险更高。在绝经后女性中,微钙化灶群与BC之间的关联与基线MD类似。
原始出处:
Shadi Azam.et al.Mammographic microcalcifications and risk of breast cancer.Brit J Cancer.2021.https://www.nature.com/articles/s41416-021-01459-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#乳腺癌风险#
40
#微钙化#
33
#钙化灶#
32
#癌风险#
37
#X线#
26