Eur Urol:根治性前列腺切除术中机器人辅助与腹腔镜手术的比较
2021-03-13 AlexYang MedSci原创
LAP-01试验旨在解决缺乏比较机器人辅助(RARP)和腹腔镜(LRP)根治性前列腺切除术高质量文献的问题。
LAP-01试验旨在解决缺乏比较机器人辅助(RARP)和腹腔镜(LRP)根治性前列腺切除术高质量文献的问题。

最近,有研究人员比较了RARP和LRP在随访3个月后的功能和肿瘤学结果。
研究是一项多中心、随机的患者单盲的对照试验,将转诊到德国四家医院进行前列腺根治术的患者随机分配(3:1)接受RARP或LRP。研究的主要结果是基于患者尿垫记录的3个月后的尿失禁恢复时间。次要结果除了肿瘤结果外,还包括随访3年的尿失禁和效用以及生活质量。研究共包括了782名患者,其中718名患者的主要终点是可评估的(547例RARP;完整分析集)。3个月时,尿失禁率的差异为8.7%,RARP更优(54% vs 46%,p=0.027)。即使调整随机分层保留神经和年龄>65岁后,RARP仍优于LRP(OR=1.40 [1.09-1.81],p=0.008)。另外,研究人员还发现了早期效能恢复的显著益处,虽然肿瘤学和发病结果相似。他们的研究没有调查不同吻合技术的影响,因此是一个局限性。
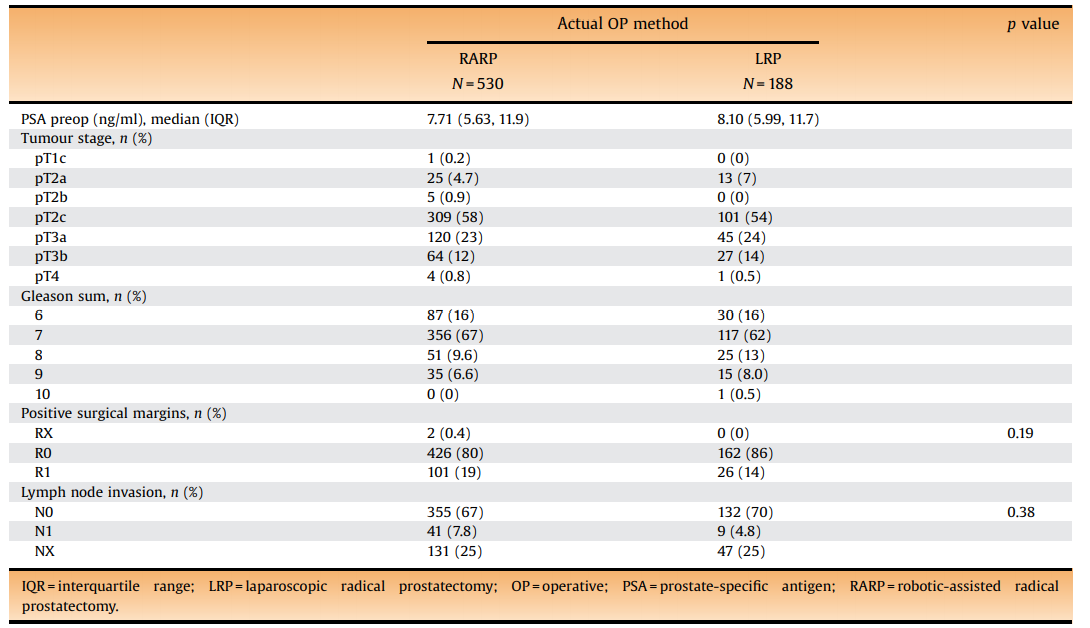
肿瘤结果
最后,研究人员指出,RARP在3个月后的尿失禁恢复情况明显更好。
原始出处:
Jens-Uwe Stolzenburg , Sigrun Holze , Petra Neuhaus et al. Robotic-assisted Versus Laparoscopic Surgery: Outcomes from the First Multicentre, Randomised, Patient-blinded Controlled Trial in Radical Prostatectomy (LAP-01). Eur Urol. Feb 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习
63
#切除术#
33
#前列腺切除#
33
#腹腔镜#
40
#机器人#
28
#机器人辅助#
39
#腹腔镜手术#
54
#机器#
35
#根治#
34