PLoS One:不同降糖药物对2型糖尿病患者动脉粥样硬化性心血管疾病风险评分的影响
2022-08-12 从医路漫漫 MedSci原创
磺酰脲类药物组合显示出LDL和甘油三酯值的显著降低。
背景:2型糖尿病是一种与短期和长期并发症相关的进行性综合征。患有二型糖尿病病的患者具有心血管并发症(如血脂异常、高血压和动脉粥样硬化性心血管事件)的高风险,并且遭受相当高的发病率和死亡率。世界范围内对T2DM患病率的预测显示,发展中国家患病率增加70%,发达国家增加20%。尽管糖尿病单一疗法有效,但大约50%的患者在3年后需要额外的药物治疗才能达到目标糖化血红蛋白(A1C) < 7% 。由于该疾病的进行性,大多数患者需要多种抗高血糖药物如磺脲类和二甲双胍来达到并维持正常血糖状态。磺酰脲类药物刺激胰腺β细胞分泌胰岛素,与血糖浓度无关,二甲双胍是一种双胍类药物,可降低肝脏葡萄糖生成,并可能增加胰岛素敏感性。DPP-4抑制剂如西他列汀可稳定肠促胰岛素肽胰高血糖素样肽-1 (GLP-1)和葡萄糖依赖性促胰岛素肽,导致血浆胰岛素水平的葡萄糖依赖性增加和随后血浆胰高血糖素水平的降低。
二甲双胍被视为一线药物,可有效控制血糖、胰岛素敏感性和体重效应。然而,二甲双胍在较长时间内效果有限,需要使用额外的药物。磺酰脲类(SU)药物经常被添加来解决这种不足。添加SU可改善血糖控制,但由于相关的不良事件,疗效并不持久。磺脲类药物与体重增加和低血糖等不良反应有关,低血糖在老年患者中比成年患者更常见。此外,一些药物通过蛋白质置换增加磺脲类药物的降血糖作用,降低肝脏代谢或减少尿液排泄需要大量的药物治疗。与其他降糖药物相比,磺脲类药物治疗还与致命性心律失常、体重增加、QT间期延长风险增加、心血管事件和死亡率增加有关。心血管并发症的风险因素是多因素的,包括抗高血糖药物对ASCVD评分、体重增加和/或低血糖的意外影响。同样,据报道,第三代磺酰脲类药物如格列美脲可诱发抗利尿激素分泌不当综合征(SIADH ),导致肾功能和肾上腺功能正常的患者出现无脱水的低钠血症(血清钠< 135 mmol/L)、肾脏钠排泄增加(尿钠> 20 mmol/L)、低血浆渗透压(< 280 mOsm/kg)和高尿渗透压(> 300 mOsm/kg)。
其他抗糖尿病药物,如格列美脲和格列吡嗪,与头晕、晕厥、头痛、恶心和血清肝酶水平升高等副作用有关。一些罕见的不良反应包括血管性水肿、休克、粒细胞缺乏症、再生障碍性贫血、双硫仑样反应、超敏反应、斑丘疹、史蒂文斯-约翰逊综合征、胆汁淤积性黄疸、肝功能衰竭、调节障碍(治疗早期)等。使用二甲双胍体重增加或低血糖的发生率相对较低。罕见不良事件乳酸酸中毒的发生率约为每1000名患者0.03例,报告死亡率为0.015例,通常与肾衰竭有关。二肽基肽酶4 (DPP-4)抑制剂是较新的抗糖尿病药物。药物不良事件包括急性肾衰竭、勃起功能障碍、周围神经病变、肾功能不全和严重关节痛。在接受基于肠促胰岛素的治疗后,患者很少报告急性胰腺炎。循证实践表明,强化血糖控制可减少并发症的发生和发展。有几种治疗方案可用于葡萄糖不耐受患者的个体化治疗计划。除了生活方式的改变,糖尿病患者通常还需要联合治疗。文献报道50%接受单一疗法糖尿病治疗的新诊断患者治疗失败。药物和药效的个体化选择是治疗成功和维持目标HbA1c水平的关键因素。
糖尿病管理的治疗目标通常集中在血清血糖水平,因此心血管事件的预防很少被遗漏或忽视。多项证据表明,与格列美脲相比,吡格列酮在减少冠状动脉粥样硬化方面具有有效作用。然而,支持口服高血糖药物在降低心血管风险方面优于首选处方的研究有限。美国食品药品监督管理局(FDA)也拒绝批准没有心血管报告风险数据的抗糖尿病药物]。因此,临床试验转向确定新的抗糖尿病药物对预防心血管事件的作用。
目的:本研究的目的是比较2型糖尿病患者口服降糖药物不同组合的临床结果。
方法:采用前瞻性、多中心、纵向、非干预性观察研究设计。在基线(0个月)时,计算临床参数,包括血糖谱、肾功能、血脂谱和心血管风险的风险评估。计算具有异质性和效应z的平均加权差(MWD ),以确定研究结束时的风险降低。
结果:共有1657人被纳入不同的队列,应答率为75.5%。患者的分布基于处方药物。G1共有513例(30.9%),G2组有217例(13.09%),G3组有231例(12.85%),G4组有384例(23.17%),G5组有312例(18.89%),G2组有217例(13.09%)(二甲双胍加格列齐特)。在基线时,所有临床和社会变量没有显著差异。组间分析显示,除了身体质量指数(p = 0.217)和表皮生长因子受体(p = 0.782)之外,使用磺脲类药物(SU)联合治疗的患者(G2和G3)的所有主要结果变量均存在显著差异。研究结果还显示,与苏(70.1% & 28.3%,p = 0.001)和DPP-4 (56.6% & 20.4%,p = 0.001)相比,的急诊和住院频率显著较高(78.16% & 30.8%)。对于ASCVD风险降低评估,报告的总体效应为z = 2.58,p = 0.001。

图1 a .在24个月的研究中身体质量指数的平均分布。在24个月的研究中体重的平均分布
表1 研究中各组的差异数据分析(24个月后)
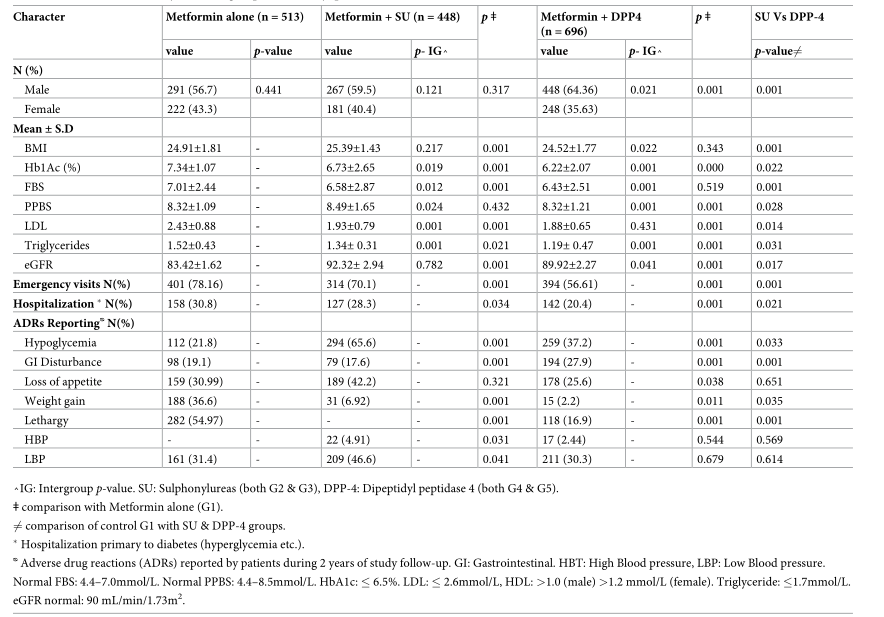
表2 ASCVD风险评估和不同队列间的比较。

结论:二肽基肽酶-4抑制剂对降低2型糖尿病患者的住院率、血脂水平以及ASCVD风险评分有显著作用,与临床合并症无关。此外,磺酰脲类药物组合显示出LDL和甘油三酯值的显著降低。
原文出处: Gillani SW, Syed Sulaiman SA, Menon V,et al.Effect of different antidiabetic medications on atherosclerotic cardiovascular disease (ASCVD) risk score among patients with type-2 diabetes mellitus: A multicenter non-interventional observational study.PLoS One 2022;17(6)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Plos one#
43
#粥样硬化性#
52
#粥样硬化#
42
#降糖药#
53
#动脉粥样硬化性心血管疾病#
66
#2型糖尿病患者#
41
#降糖药物#
39
#疾病风险#
42
#糖尿病患者#
42
#硬化性#
44