Neurosurgery:动脉瘤蛛网膜下腔出血后持续输注替罗非班
2020-02-22 杨中华 脑血管病及重症文献导读
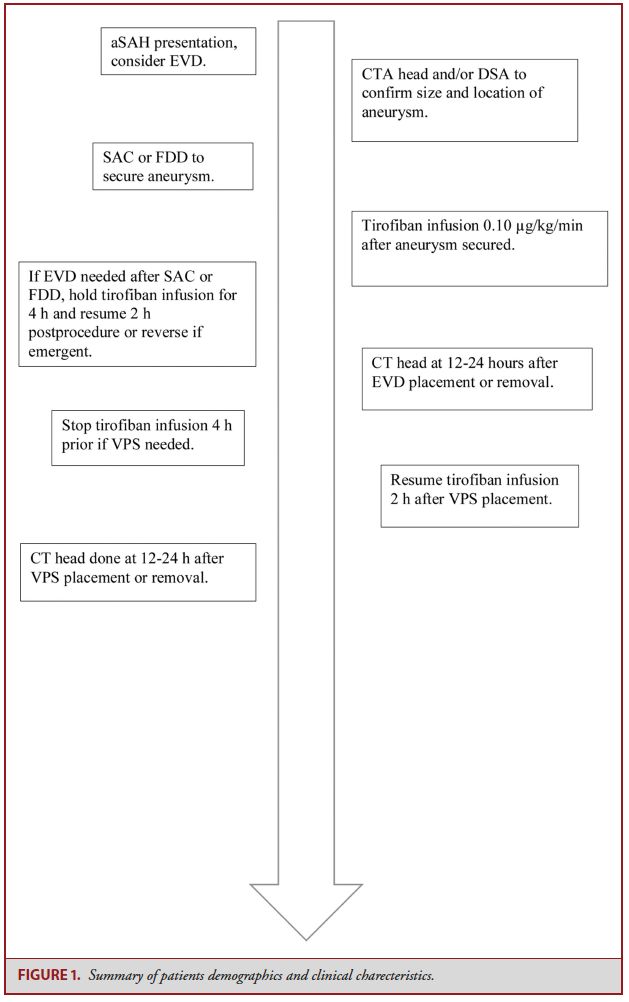
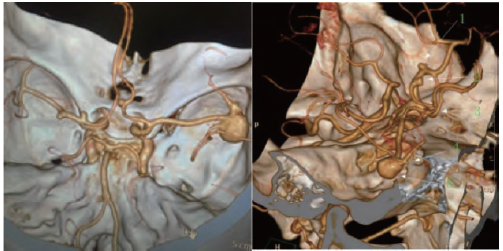
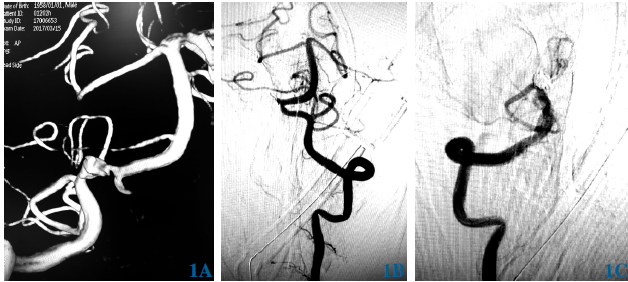
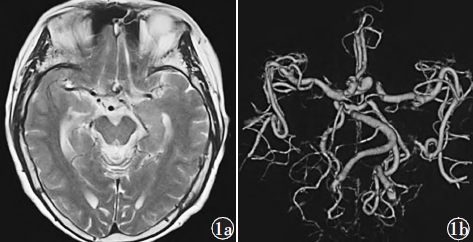
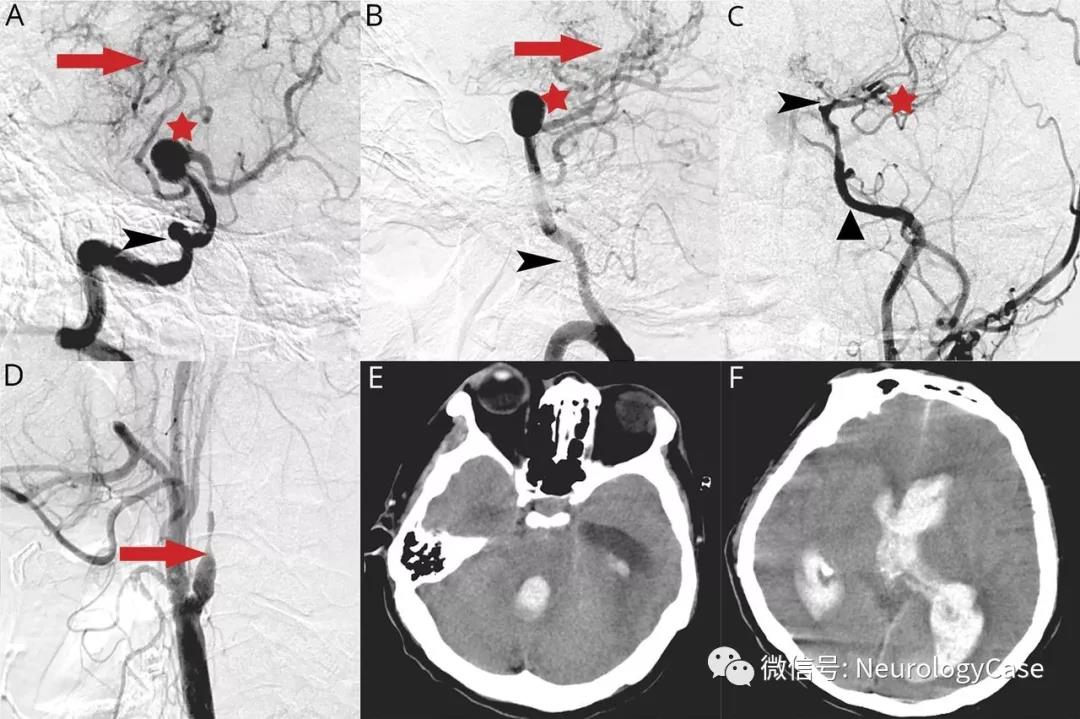
2019年12月来自美国的Kaustubh Limaye等在NEUROSURGERY上公布了他们的研究结果,目的在于评价支架辅助弹簧圈栓塞(SAC)或血流分流装置(FDD)治疗的破裂动脉瘤并且需要脑室外引流(EVD)或脑室腹膜分流(VPS)的患者,长时间持续输注替罗非班单一抗血小板药物的安全性和有效性。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#蛛网膜#
48
#GER#
51
#surgery#
42
#动脉瘤蛛网膜下腔出血#
47
#ROS#
52