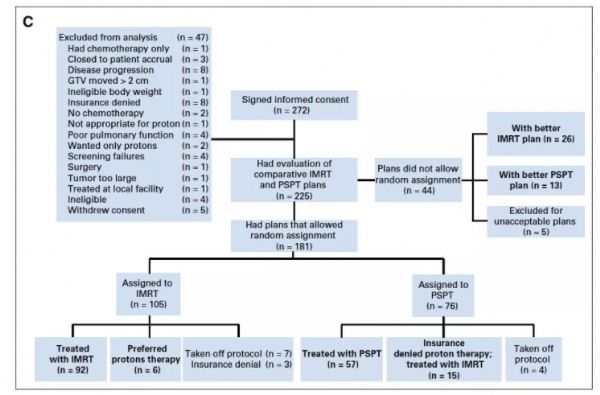
JCO:局部晚期NSCLC,质子和光子放疗,谁主沉浮?
2018-01-07 宋小编 肿瘤资讯
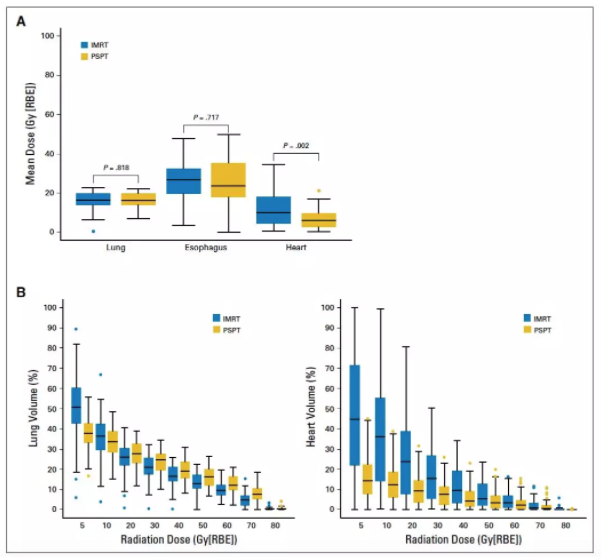
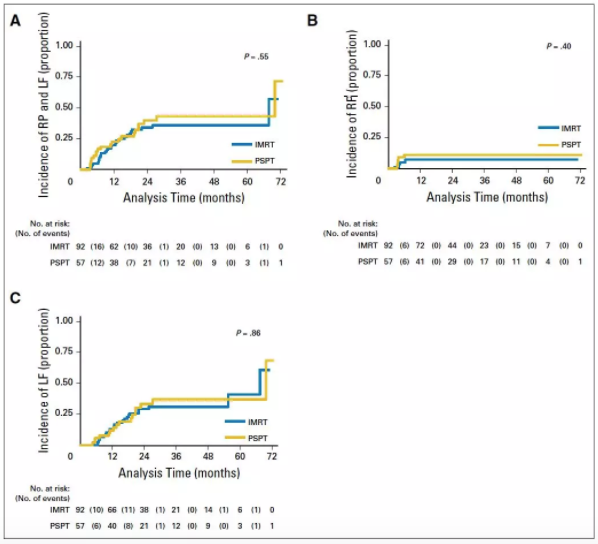
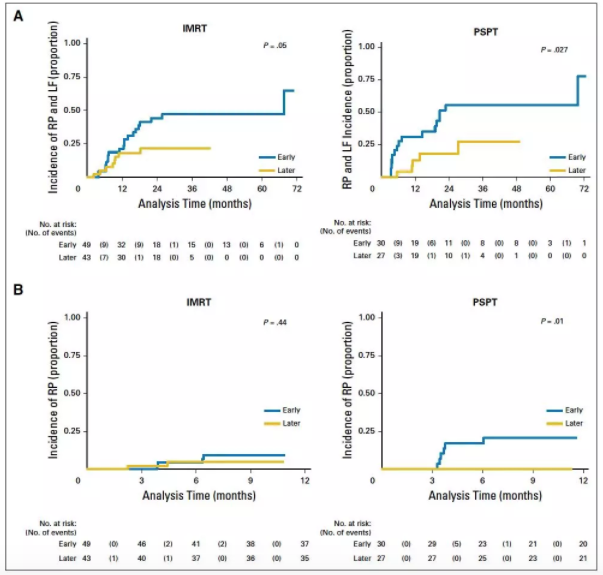
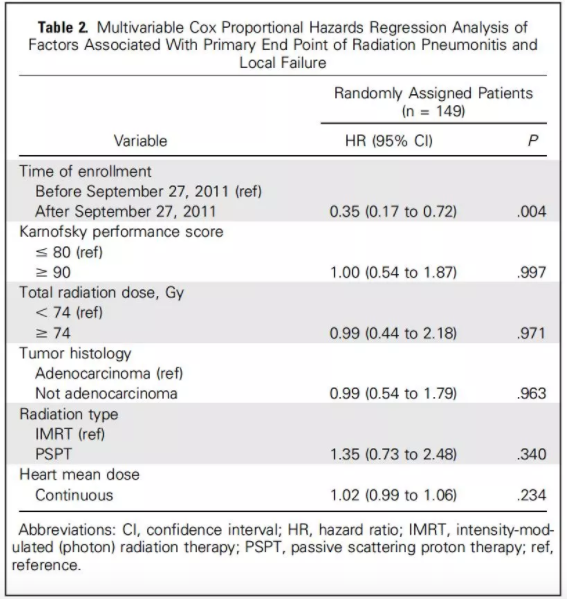
同步放化疗是局部晚期NSCLC的标准治疗。目前临床上多采用调强放疗(光子放疗),但仍有部分患者可能出现严重的放射性肺炎。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JCO#
39
#局部晚期#
42
#局部#
53
#晚期NSCLC#
35
#光子放疗#
42
henhao
70