Brit J Cancer:循环肿瘤细胞与神经内分泌肿瘤患者骨转移的关系
2019-01-14 xing.T MedSci原创
由此可见,CTC与NETs患者的骨转移相关。CXCR4可能参与CTC的向骨性,并提供了减少骨骼发病率的治疗靶点。
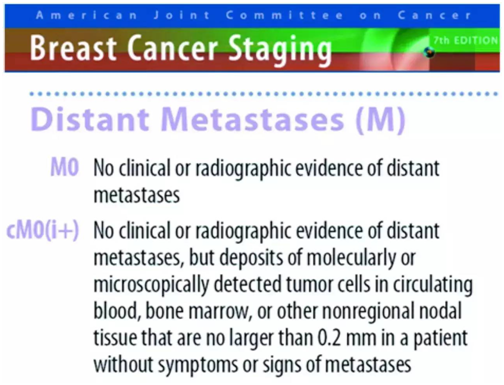
骨转移与神经内分泌肿瘤(NETs)患者的预后较差有关。肿瘤过度表达C-X-C趋化因子受体4(CXCR4)似乎可预测骨骼受累情况。近日,肿瘤领域权威杂志British Journal of Cancer上发表了一篇研究文章,研究人员分析了循环肿瘤细胞(CTC)和CXCR4在CTC上的表达作为骨骼侵袭的潜在预测因子。
研究人员通过CellSearch分析了来自患有转移性支气管、中肠或胰腺NET(pNET)患者的血液。在匹配的福尔马林固定的石蜡包埋(FFPE)样品上进行CXCR4免疫组织化学检查。
该研究共招募了254名患者,其中121名中肠NET患者和119名pNET患者,其中分别有51%和36%的患者具有可检测到的CTC。在30%的中肠NET患者和23%的pNET患者中报告了骨转移,并且与CTC存在显著相关性(p=0.003和p<0.0001)。在40名患者的亚组中,85%的具有CTC患者CTC表达CXCR4阳性。骨转移患者中CXCR4表达阳性的CTC比例为56%,而没有骨转移的患者为35%(p=0.18)。在匹配的FFPE组织上对CXCR4染色显示出与CTC上CXCR4表达相关的趋势(p=0.08)。
由此可见,CTC与NETs患者的骨转移相关。CXCR4可能参与CTC的向骨性,并提供了减少骨骼发病率的治疗靶点。
相关资源:高级别胃肠内分泌癌预后评分(GI-NEC)
原始出处:
Francesca M. Rizzo,et al.Circulating tumour cells and their association with bone metastases in patients with neuroendocrine tumours. British Journal of Cancer. 2019. https://www.nature.com/articles/s41416-018-0367-4
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#内分泌肿瘤#
36
#分泌#
30
#神经内分泌#
33
认真学习,不断进步,把经验分享给同好。点赞了!
49
#肿瘤细胞#
28
#肿瘤患者#
29
#循环肿瘤细胞#
24
谢谢分享,学习了
45
看看
57
学习了
56