J Am Coll Cardiol:心率对主动脉中心压力和血流动力学的影响
2020-07-31 MedSci原创 MedSci原创
最近的分析表明,β-受体阻滞剂在减少心血管事件方面不如其他降血压(BP)疗法有效。关于这种获益不足的机制,特别是β-受体阻滞剂降低HR的作用,一直有很多争论。
最近的分析表明,β-受体阻滞剂在减少心血管事件方面不如其他降血压(BP)疗法有效。关于这种获益不足的机制,特别是β-受体阻滞剂降低HR的作用,一直有很多争论。
从肱动脉压力和桡动脉脉搏波分析中得出2073名患者的中心压力,并记录了7146次测量结果,并对其进行了长达4年的随访分析。
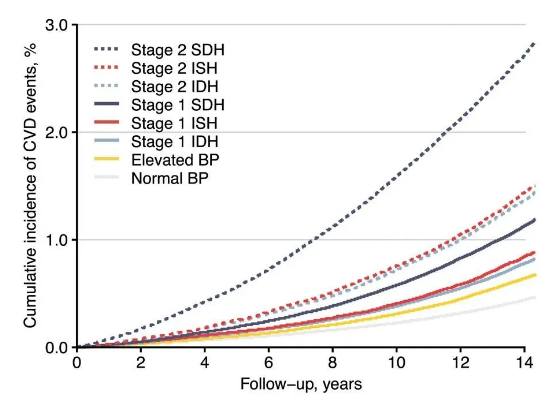
结果显示,HR对肱动脉收缩压或脉搏压没有影响;然而,HR与主动脉中央收缩压和脉搏压之间存在高度明显的反向关系(P <0.001)。这取决于HR和增强指数之间的强烈反比关系,表明较低HR时波反射增加。经肱动脉血压校正后的多元回归显示,HR是中心压力的主要决定因素。此外,HR和肱动脉血压占中心收缩压和脉搏压力变异的92%。因此,校正HR后,主动脉中心压的药物相关差异明显减弱。
综上所述,该研究结果表明,当比较基于β-受体阻滞剂的治疗和其他降压策略时,β-受体阻滞剂的HR降低是造成肱动脉压每单位变化的中央主动脉压降低效果较差的主要机制。
原始出处:
Bryan Williams, Peter S Lacy, et al., Impact of heart rate on central aortic pressures and hemodynamics: analysis from the CAFE (Conduit Artery Function Evaluation) study: CAFE-Heart Rate. J Am Coll Cardiol. 2009 Aug 18;54(8):705-13. doi: 10.1016/j.jacc.2009.02.088.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#血流动力#
32
#Coll#
30
#Cardiol#
36
#血流动力学#
0
#主动脉#
34
#心率#欣宇可能是被大家忽视的,也许他很有价值。
0
好文章共享,学习了
97