Hepatology:乙肝纳米疫苗εPA-44可明显提高CHB患者的HBeAg血清学转换率
2021-08-18 Nebula MedSci原创
短时间持续予以900 μg εPA-44单一疗法可较安慰剂明显提高HLA-A2阳性的进展性CHB患者的HBeAg血清学转换率
慢性乙肝(CHB)患者可采用抗病毒药物降低其体内的HBV DNA载量;但是,HBeAg血清学转换(即HBeAg转阴且抗-HBeAb转阳)率仍然很低。一项临床试验评估了新开发的以脂质体为基础的纳米脂肽疫苗εPA-44用于CHB患者的效果和安全性。
8月15日在肝病领域顶级杂志Hepatology 在线发表陆军军医大学吴玉章教授团队原创的模拟抗原乙肝治疗性疫苗(ɛPA-44,中文名称伊帕)II期临床试验结果。该研究由北京大学附属人民医院等国内顶尖15家临床中心共同完成。论文通讯作者是陆军军医大学的吴玉章教授,第一作者为北京大学附属人民医院魏来教授、重庆国际免疫研究院赵婷婷教授、陆军军医大学张记博士等。从研究注册信息来看,本研究从2009年开始。
基于II期临床试验结果,伊帕已经获得了国家药品监督管理局的III期临床试验批件,已经开始多中心的III期临床试验(ChiCTR2100043708)。
这是一项在中国的15家医疗中心开展的双阶段的2期试验,包括一项为期76周的随机、双盲、安慰剂为对照的试验(1阶段)和一项为期68周的开放标签的扩展试验(2阶段)。在1阶段,360位HLA-A2阳性、HBeAg阳性的患者被随机均分至两组,接受6剂皮下注射600 μg或900 μg εPA-44(第0/4/8/12/20和28周),或安慰剂。在2阶段,183位患者接受了 900 μg εPA-44延长治疗,26位患者在没有进一步治疗的情况下观察到复发。主要终点是76周时HBeAg血清学转换的患者比例。
研究流程
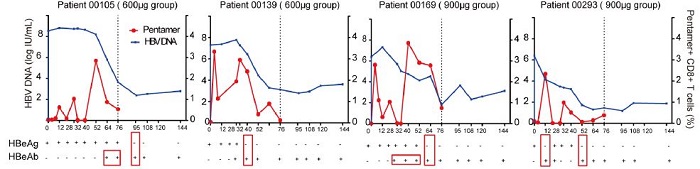
在76周时,接受900 μg εPA-44治疗的患者的HBeAg血清学转换率明显高于安慰剂组(38.8% vs 20.0%;p=0.002)。对于HBeAg血清学转换、ALT正常化和HBV DNA <2000 IU/mL的综合终点,76周时,与安慰剂相比,600或900 μg εPA-44干预治疗综合终点的实现率均显著高于安慰剂组(18.1% vs 14.3% vs 5.0%;p值分别是0.002和0.02)。在2阶段研究中,接受900 μg εPA-44治疗的20位患者,无一发生血清学复发。最后,εPA-44的安全性与安慰剂的相当。
4位患者的HBV DNA载量变化
值得注意的是,在12名干扰素或/和核苷(酸)类似物治疗无效的病人中,有5名(41.7%)病人实现了HBeAg 血清转换并ALT 复常,这表明伊帕可能对干扰素和核苷(酸) 类似物治疗无效的病人有效。本研究中安慰剂组的e抗原血清转换率为20.2%,高于慢乙肝病人的自然转阴率,但与上海复旦大学闻玉梅院士团队报道的YIC(乙克)治疗性疫苗的III期临床试验的安慰剂组的e抗原血清学转阴率相当(21.9%)。 作者解释,这可能主要是由于该研究中使用的安慰剂(空脂质体颗粒)具有激活固有免疫应答的功能有关。试验中,有病人接近实现慢乙肝的功能治愈。乙肝被称为国病。伊帕作为我国科学家自主发明的创新生物制品,正在进行多中心、随机、双盲双模拟、阳性药对照的III期临床试验 (ChiCTR2100043708)。
综上所述,短时间持续予以900 μg εPA-44单一疗法可较安慰剂明显提高HLA-A2阳性的进展性CHB患者的HBeAg血清学转换率。
原始出处:
Wei Lai,Zhao Tingting,Zhang Ji et al. Efficacy and Safety of a Nanoparticle Therapeutic Vaccine in Patients with Chronic Hepatitis B: A Randomized Clinical Trial.[J] .Hepatology, 2021, https://doi.org/10.1002/hep.32109
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#HBeAg#
48
#EPA#
35
#CHB#
0
#血清学#
38
感谢
0
不错
55
不错学习了
62