JACC:中度主动脉瓣狭窄分级和血流梯度不一致的发生率和预后意义
2022-08-11 MedSci原创 MedSci原创
低血流、低梯度模式占不一致病例的重要比例,并与死亡风险增加有关
重度主动脉瓣狭窄 (AS) 分级不一致的预后影响是众所周知的。但是,不同的血流梯度模式在中度AS中的流行情况及其预后意义尚不清楚。
本研究旨在探讨不同血流梯度模式在中度AS患者中的发生情况及预后意义。
招募主动脉瓣面积>1.0及≤1.5 cm2的中度AS患者,并根据经瓣膜平均梯度 (MG)、卒中容积指数 (SVi)、左心室射血分数 (LVEF) 分为4组:一致型中度AS (MG≥20 mm Hg) 和包括3个亚组的不一致型中度AS:正常血流、低梯度中等AS (MG<20 mm Hg、SVi≥35 mL/m2、LVEF ≥50%);“矛盾的”低血流、低梯度中度AS (MG<20 mm Hg、SVi<35 mL/m2、LVEF ≥50%) 和“经典的”低血流、低梯度中度AS (MG<20 mm Hg、LVEF <50%)。主要终点是全因死亡率。
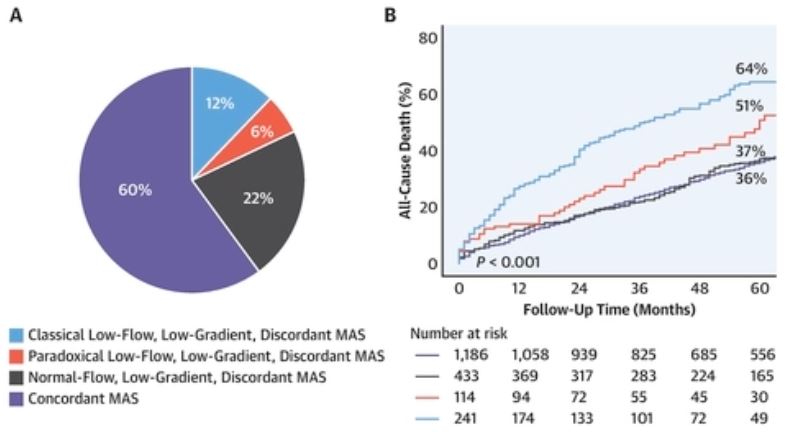
不同类型患者的占比及其全因死亡的发生率
在1974位中度AS患者(平均73±10岁,51%的男性)中,788位(40%)属于不和谐的分级,这些患者的死亡率明显高于一致型中度AS患者(p<0.001)。在多变量分析中,“矛盾的”低血流、低梯度中度AS(HR 1.458,p=0.014)和“经典的”低血流、低梯度中度AS(HR 1.710, p<0.001)都是全因死亡的独立预测因素,但正常血流、低梯度中度AS型无此相关性。
总之,在中度AS患者中,分级不一致 (40%) 的发生率较高。低血流、低梯度模式占不一致病例的重要比例,并与死亡风险增加有关。该研究发现强调了对不一致型中度AS患者加强监测的需要。
原始出处:
Stassen J, Ewe S, Singh G, et al. Prevalence and Prognostic Implications of Discordant Grading and Flow-Gradient Patterns in Moderate Aortic Stenosis. J Am Coll Cardiol. 2022 Aug, 80 (7) 666–676. https://doi.org/10.1016/j.jacc.2022.05.036
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
48
#发生率#
43
#ACC#
41
#主动脉瓣#
31
#主动脉#
51
#预后意义#
54