糖尿病与心血管病之间存在着密切的内在联系,二者互为高危人群。2001 年美国国家胆固醇教育计划成人治疗指南Ⅲ(NCEP-ATP Ⅲ)指出:糖尿病是冠心病的等危症。2007 年,美国心脏病学院甚至发出了“糖尿病就是心血管病”的呼声。提高对糖尿病患者冠状动脉病变和介入治疗的认识,以及加强经皮冠状动脉介入治疗(PCI)术后对血糖等危险因素的管理,对于最大程度地改善患者的预后具有重要意义。
然而,糖尿病合并慢性冠心病(CCD)患者中,目前还不清楚在药物治疗的基础上增加侵入性管理是否能改善结果。为了明确上述结果,来自纽约大学的专家开展了ISCHEMIA试验,结果发表在Circulation杂志上。
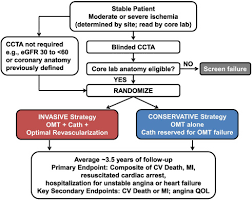
ISCHEMIA试验(ISCHEMIA和ISCHEMIA CKD)将CCD患者随机分为侵入性治疗(药物治疗+血管造影和血管重建)或保守性治疗(单纯药物治疗,如果药物治疗失败,则进行血管重建)。在没有观察到试验的特定效果后,队列被合并。糖尿病的定义是有病史,HbA1c≥6.5%,或使用降糖药物。主要结果是全因死亡或心肌梗死(MI)。使用贝叶斯方法评估了侵入性管理对死亡或MI的影响的异质性,以防止对糖尿病患者与非糖尿病患者以及临床(女性性别和胰岛素使用)和解剖学特征(冠状动脉疾病[CAD]严重程度或左心室功能)的糖尿病亚组的治疗效果的随机高或低估计。
结果在有完整基线数据的5900名参与者中,中位年龄为64岁,四分位数范围(IQR)[57-70],24%为女性,估计肾小球滤过率中位数为80ml/min/1.73m。在2553名(43%)患有糖尿病的参与者中,HBA1c百分比的中位数为7%,30%接受胰岛素治疗。
总的来说,患有糖尿病的参与者的死亡或MI的危险增加了49%(HR 1.49;95% CI:1.31-1.70)。在中位3.1年的随访中,调整后的无事件生存率为0.54,有糖尿病与无糖尿病的患者为0.66--有糖尿病的参与者的无事件生存率绝对下降12%。胰岛素治疗的女性和男性糖尿病患者的调整无事件生存率分别为0.52和0.49。
综上,尽管死亡或MI的风险较高,但与单纯的初始药物治疗相比,CCD患者并没有从常规侵入性管理中获得更多的益处。
参考文献:
Outcomes of Participants with Diabetes in the ISCHEMIA Trials. https://doi.org/10.1161/CIRCULATIONAHA.121.054439
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#治疗结局#
43
谢谢分享。很有用
41
学习了
68
xuexile
72
学习了
69