Aliment Pharmacol Ther:炎症性肠病诊断前后的合并症
2021-08-30 MedSci原创 MedSci原创
Charlson共病指数(CCI)中各组成部分疾病的诊断前相对比率(RR)和诊断后风险比(HR)。
常见的炎症性肠外疾病与炎症性肠病(IBD)合并症包括炎症性关节炎,如血清阴性脊柱关节病,以及炎症性皮肤病,如坏疽性脓皮病、结节性红斑,原发性硬化性胆管炎和炎症性眼病,如葡萄膜炎。精神疾病如抑郁和焦虑、骨质疏松和静脉血栓代谢疾病在IBD患者中也比普通人群更常见;在IBD治疗过程中注意这些情况出现的可能性被认为是高质量IBD治疗的必要指标。合并症是炎症性肠(IBD)病程发展的重要预测因素。本研究目的旨在通过对IBD患者的队列研究,确定Charlson共病指数(CCI)中各组成部分疾病的诊断前相对比率(RR)和诊断后风险比(HR)。
在这项研究中,研究纳入曼尼托巴大学IBD流行病学数据库中1984年4月1日至2018年3月31日期间所有IBD的曼尼托巴患者以此匹配对照。对所有门诊医生索赔和出院摘要进行搜索(CCI组成疾病的诊断代码),将一些疾病归为一组,因此评估了12种情况。研究报告了IBD之前这些病症的RR,以及IBD之后这些诊断的发生率。我们使用Cox比例风险回归报告诊断后HR。针对Bonferroni校正调整了置信区间。
研究共纳入9247例IBD(4253例CD,4994例UC)和85691例对照。诊断IBD的中位年龄为36(25-52),CD患者(33岁[23-49])明显低于UC患者(39岁[27-54],P<0.0001)。其中47%的IBD病例是男性。IBD病例和对照组的社会经济因素指数得分相似(表1)。

表1实验组和对照组的患者特征
总体上,rr与HRs高度相关(r=+0.69,P=0.013)。CD(r=+0.69,P=0.013)和UC(+0.71,P=0.0094)表现出相似的模式。在疾病类型间比较时,CD组RR(P=0.012)和HR(P=0.0015)高于UC组。男性和女性的RR和HR总体上没有显著差异。
IBD前诊断合并症:除糖尿病和痴呆外,所有合并症的预诊断均增加(表2)。
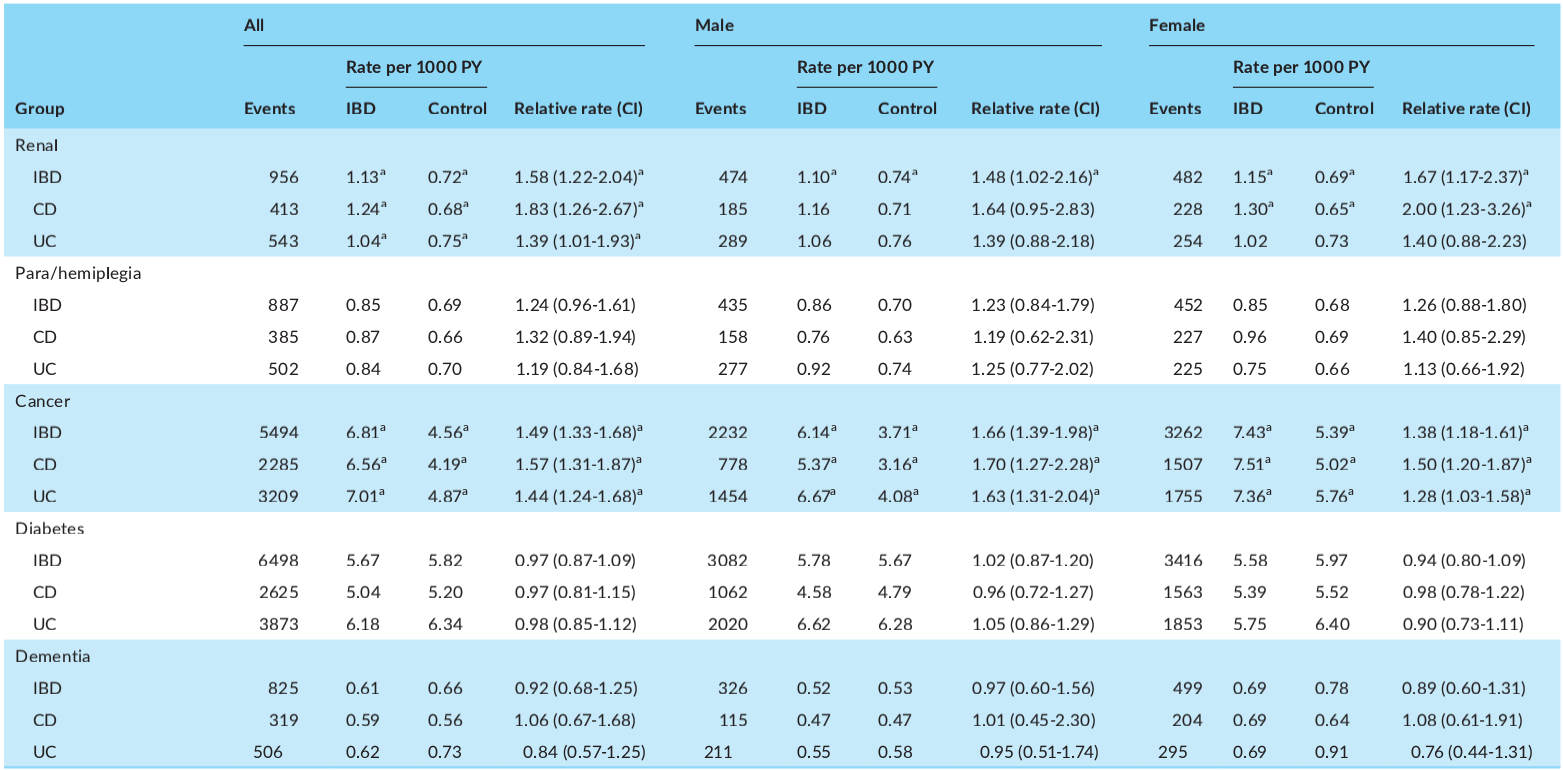
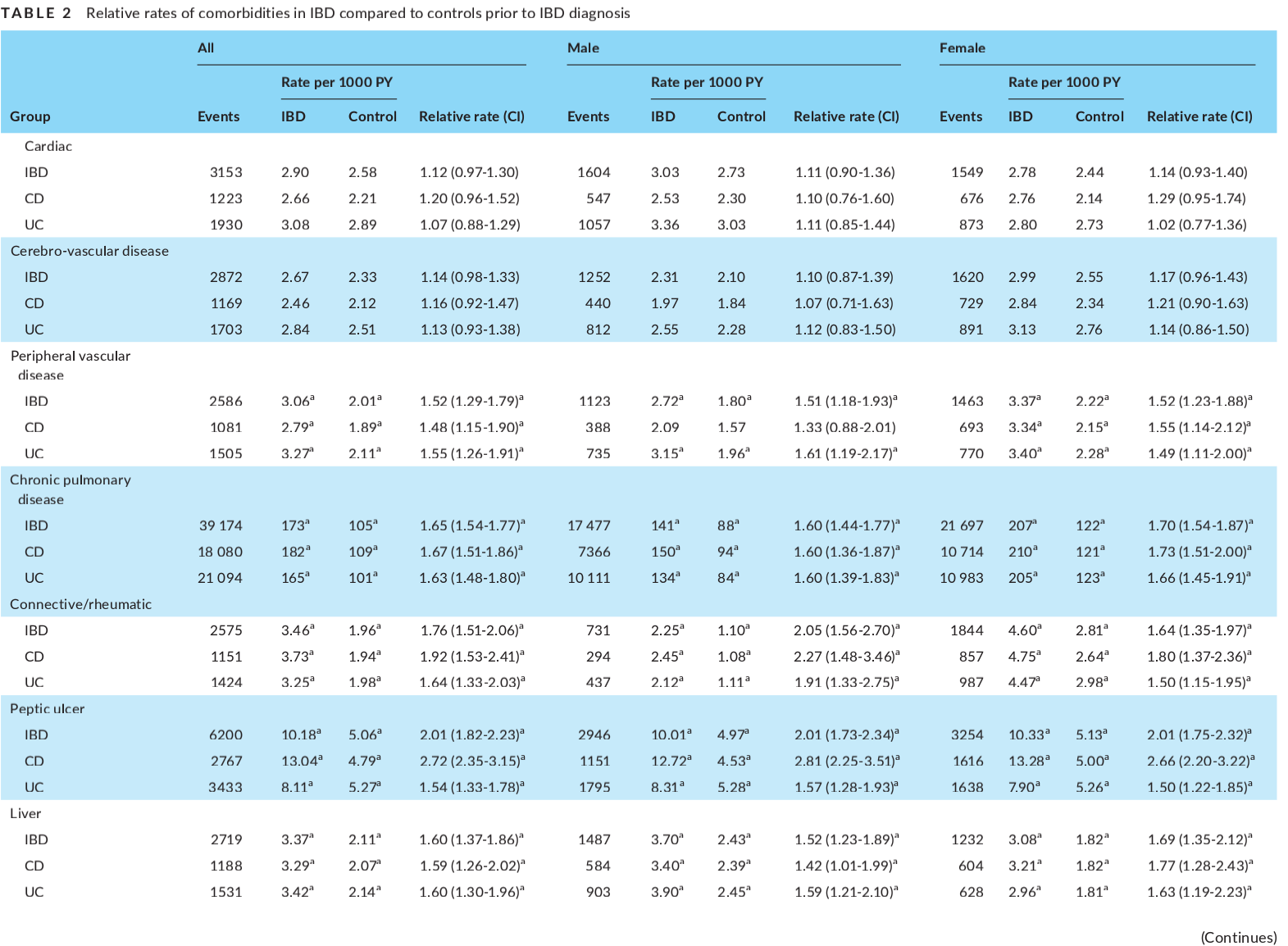
表2诊断IBD前IBD患者与对照组的合并症相对发生率
在所有合并症中,消化性溃疡的预诊断RR最高[RR=2.01,CI1.82,2.23]。对于所有心脏、结缔组织疾病/风湿病、消化性溃疡和肾脏疾病,乳糜泻患者的RR高于UC患者。对于周围血管疾病、慢性肺病、肝病和癌症,CD和UC的增加幅度相似。在脑血管疾病、截瘫/偏瘫、糖尿病和痴呆患者中,CD或UC均无增加。脑血管病女性的RR高于男性,而其他所有合并症的RR在性别上没有差异。
与对照组相比,在IBD诊断之前,心血管疾病、外周血管疾病、慢性肺病、结缔组织病/风湿病、肾病、肝病、消化性溃疡病和癌症的RR均有所增加。IBD诊断后所有合并症均增加。克罗恩病患者痴呆的HR增加是一个令人担忧的新发现。与截瘫/偏瘫的增加的关联是出乎意料的。对于除糖尿病以外的所有合并症,IBD的诊断年龄均小于控件。
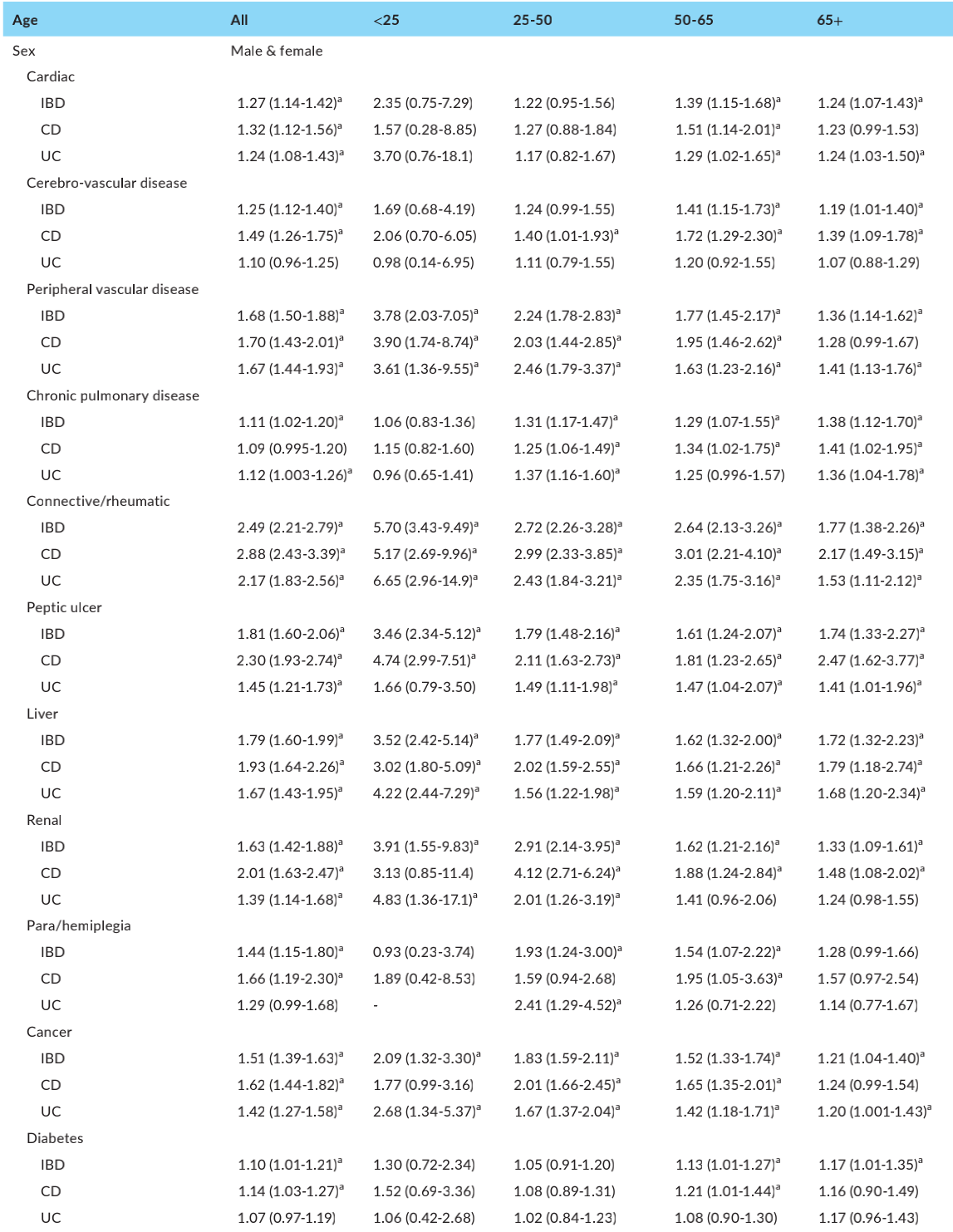
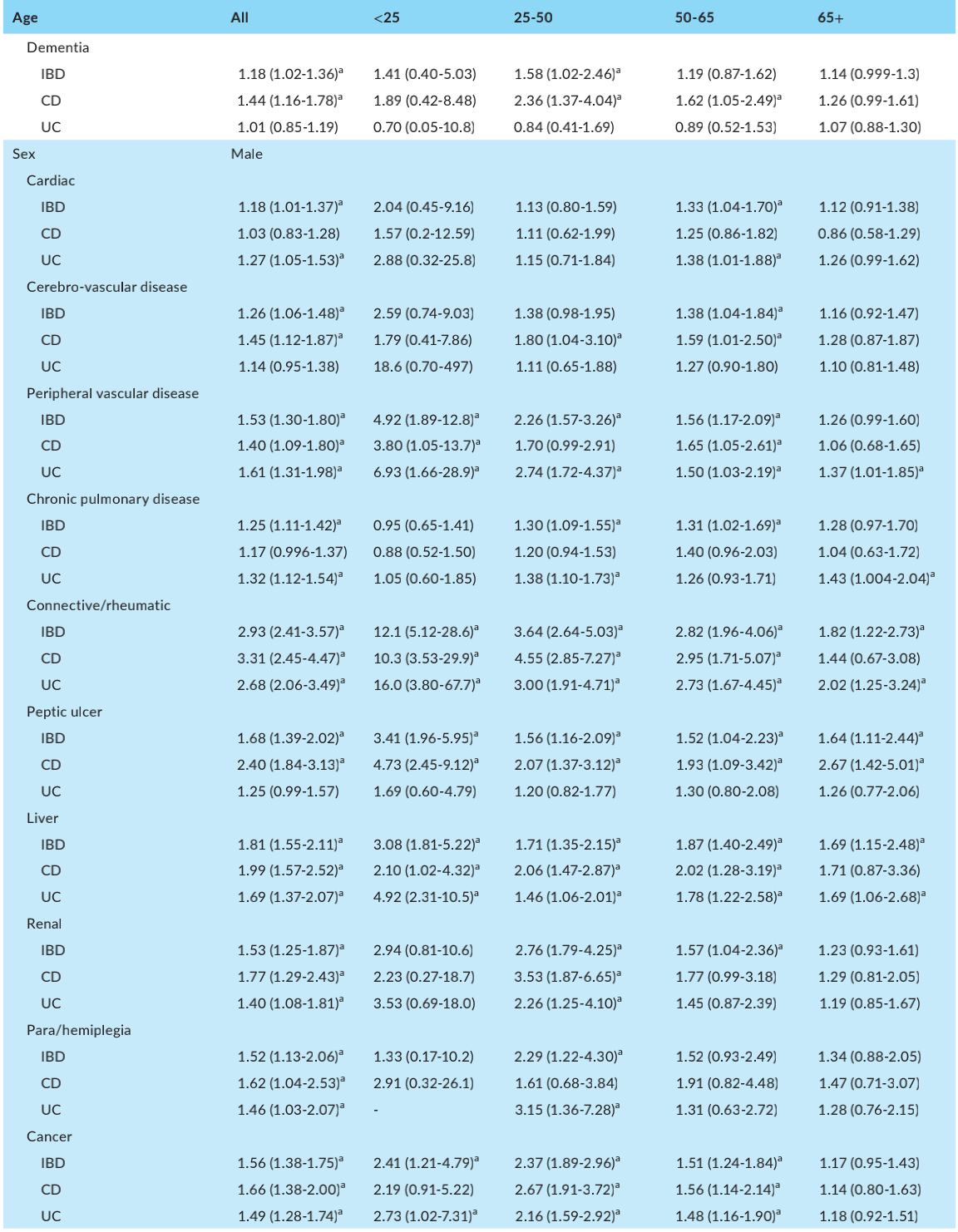
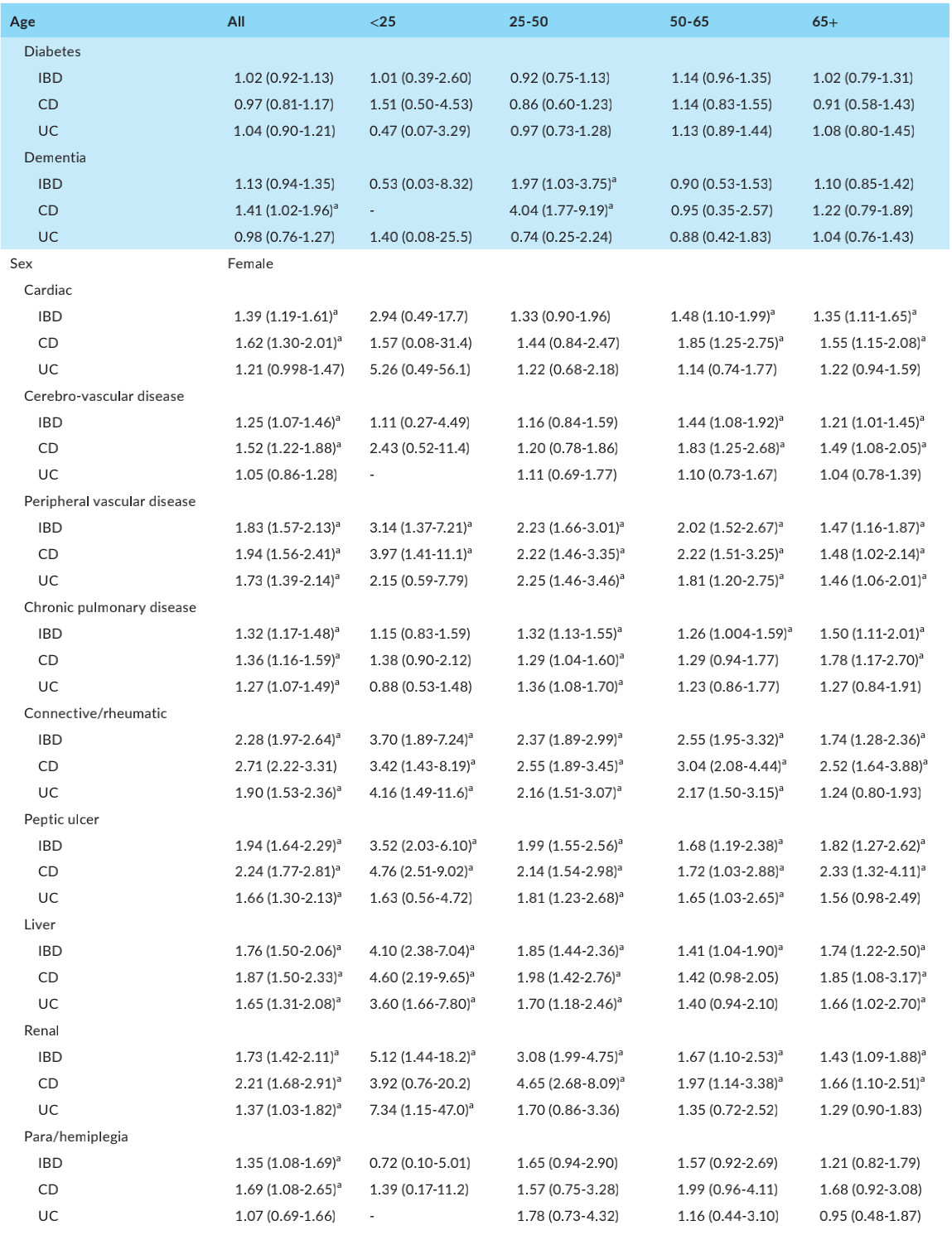

表3:IBD诊断后共病疾病的总体危险比以及按年龄组和性别分列的危险比
IBD后诊断合并症:所有的合并症均在IBD诊断后增加(表3)。脑血管病(1.49(1.26-1.75))、截瘫/偏瘫(1.66CI(1.19-2.30))、糖尿病(1.14(CI1.03-1.27))和痴呆(1.44(CI1.16-1.78))患者的HR显著增加,但UC患者的HR均无明显增加。对于慢性肺部疾病,UC增加显著[1.12(1.003-1.26)],而CD增加不显著。在所有其他合并症中,CD和UC患者的HR均明显增加,但消化性溃疡和肾病患者的HR增加幅度更大。诊断后HR增加最多的是结缔组织病/风湿病[HR = 2.49 (CI 2.21-2.79)],尤其是结缔组织CD中的疾病/风湿性疾病[HR = 2.88 (CI 2.43-3.39)]。
总之,与没有IBD的患者相比,患有IBD的人有更高的合并症负担。 IBD患者的最佳护理计划应包括对其他所有其他器官系统合并症的评估。
原始出处
Bernstein CN, Nugent Z, Shaffer S, Singh H, Marrie RA. Comorbidity before and after a diagnosis of inflammatory bowel disease. Aliment Pharmacol Ther. 2021 Sep;54(5):637-651. doi: 10.1111/apt.16444. Epub 2021 Jun 22. PMID: 34156724.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Pharmacol#
35
#pharma#
33
#MAC#
36
学习了
61
#Pharm#
30
#合并症#
26
#炎症性#
21