Int J Pediatr Otorhinolaryngol:射频消融鼻甲成形术可改善儿科患者的嗅觉
2021-11-09 AlexYang MedSci原创
评估了首次接受TRA小儿患者的嗅觉变化情况。
嗅觉对儿童的充分发育至关重要。儿童的嗅觉丧失有着不同的起因,其中最常见的是传导性原因,即鼻腔阻塞使气味无法到达嗅觉上皮细胞。目前,已证明鼻炎和鼻甲肥大会削弱小儿患者的嗅觉。对于这些患者的鼻炎,常见的治疗方法是鼻甲射频消融术(TRA)。尽管该领域的研究力度很大,但迄今为止还没有研究对接受鼻甲手术儿童的嗅觉进行评估。
近期,来自西班牙的研究人员在《Int J Pediatr Otorhinolaryngol》上发表文章,评估了首次接受TRA小儿患者的嗅觉变化情况。
研究为前瞻性的非受控干预性临床试验设计。在一家三级转诊医院选取了两组4-15岁的儿童,并在术前和术后1、3、6个月分别用通用嗅觉测试(U-Sniff)、酒精嗅觉测试(AST)和嗅棒阈值测试(SST)进行评估。队列A包括仅接受TRA的儿童。队列B由进行过腺样体切除术和TRA的儿童组成。此外,还包括了健康对照组,并按性别和年龄配对,并进行嗅觉测试。
研究共纳入了81名参与者,平均年龄为10.31±2.56岁。53名患者接受TRA,28名患者接受相关的腺样体切除术。结果发现,尽管U-sniff评分在术后有改善的趋势,但没有统计学上的显著差异。然而,SST和AST测量结果具有统计学上的显著差异,包括手术后1个月、3个月和6个月。
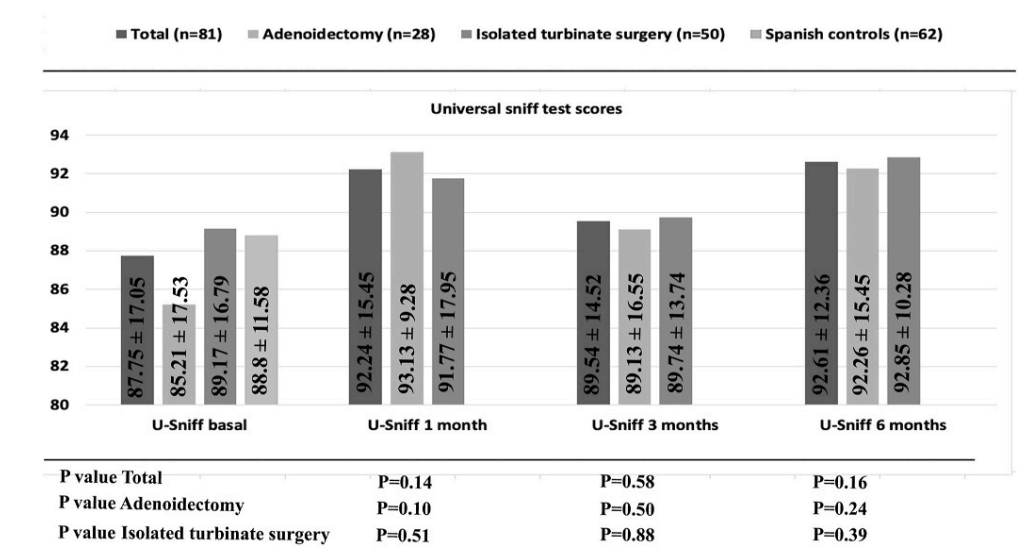
术前和术后1、3、6个月的U-Sniff测试结果
综上所述,TRA或TRA与腺样体切除术联用,可改善嗅觉阈值得分,但对鉴别任务没有明显影响。
原始出处:
Christian Calvo-Henriquez, Franklin Mariiño-Sánchez, Jerome R Lechien et al. Radiofrequency ablation turbinoplasty improves the sense of smell in pediatric patients: A prospective study. Int J Pediatr Otorhinolaryngol. Nov 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#儿科患者#
44
#成形术#
35
#PE#
48
#DIA#
45
#射频消融#
49
#消融#
34
学习赚积分
67