Lancet Respirat:Savolitinib在METex14跳跃变异阳性的中国肺癌患者中的疗效可期!
2021-06-23 Nebula MedSci原创
萨沃替尼用于携带METex14跳跃变异的肺肉瘤样癌和其他NSCLC亚型患者的治疗活性可期,安全性可控
Savolitinib(萨沃替尼)是一种选择性MET酪氨酸激酶抑制剂。本研究旨在评估萨沃替尼用于MET外显子14跳跃变异阳性(METex14 阳性)的肺肉瘤样癌和其他非小细胞肺癌 (NSCLC) 亚型患者的活性和安全性。
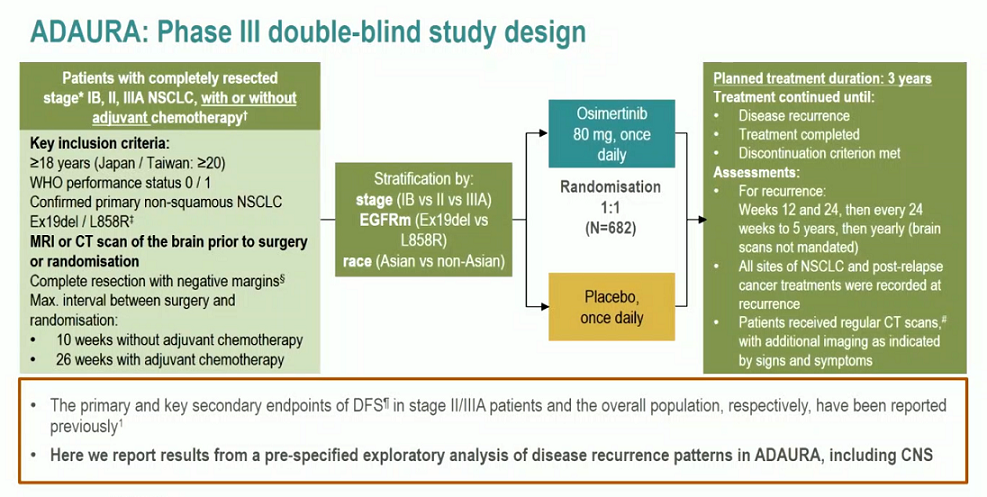
这是一项在中国的32家医院开展的多中心、单臂、开放标签的2期研究,招募了年满18岁的局部晚期或转移性METex14阳性的肺肉瘤样癌或其他NSCLC亚型患者,要求受试患者对一种或多种标准治疗的毒性不耐受或治疗后出现进展,或不适用标准疗法,且未接受过MET抑制剂治疗、有可测量的病灶。每日予以受试患者萨沃替尼 600 mg(体重≥50 kg)或400 mg(体重<50 kg)口服,直达病情进展、死亡、不可耐受的毒性、开始其他抗肿瘤治疗或患者撤出研究。在开展治疗1年内,每6周进行一次影像评估,一年后,每12周评估一次。主要终点是客观缓解率。
2016年11月8日-2020年8月3日,共筛查到84位METex14跳跃变异阳性的患者,其中70位被招募入组,接受萨沃替尼治疗。61位患者接受了独立审查委员会 (IRC)评估(肿瘤缓解可评估队列)。
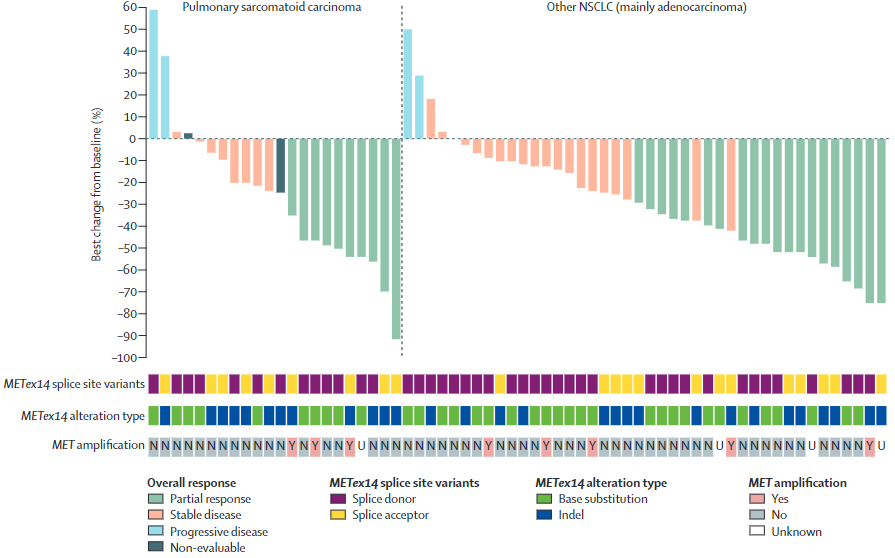
肿瘤病灶的最大缓解情况
中位随访了17.6个月(IQR 14.2-24.4)时,在肿瘤缓解可评估队列中,IRC评估的客观缓解率为49.2%(30/61),该值在整个分析队列中为42.9%(30/70)。
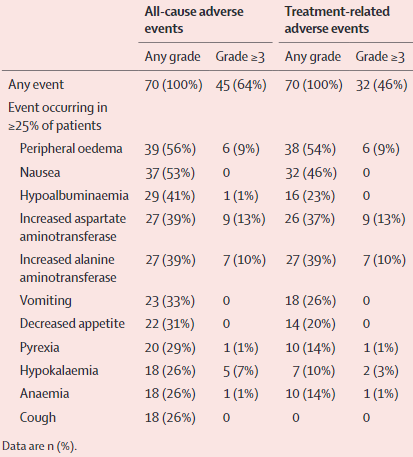
不良反应事件
接受萨沃替尼治疗的70位患者都至少报告了一种治疗相关的不良反应事件。32位(46%)患者报告了3/4级的治疗相关的不良反应事件,最常见的是天冬氨酸转氨酶升高(n=9)、丙氨酸氨基转移酶升高(n=7)和外周水肿(n=6)。17位(24%)患者报告了与治疗相关的严重不良反应,最常见的是肝功能异常(n=3)和超敏反应(n=2)。一位肺肉瘤样癌患者死于肿瘤溶解综合征,经评估认为与萨沃替尼相关。
总而言之,萨沃替尼用于携带METex14跳跃变异的肺肉瘤样癌和其他NSCLC亚型患者的治疗活性可期,安全性可控。未来萨沃替尼或可成为这类患者的治疗选择。
原始出处:
Shun Lu, et al. Once-daily savolitinib in Chinese patients with pulmonary sarcomatoid carcinomas and other non-small-cell lung cancers harbouring MET exon 14 skipping alterations: a multicentre, single-arm, open-label, phase 2 study. The Lancet Respiratory. June 21, 2021. https://doi.org/10.1016/S2213-2600(21)00084-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Lancet#
27
#肺癌患者#
44
#MET#
32
#变异#
32
谢谢梅斯提供这么好的信息,学到很多
52
顶刊就是不一样,质量很高,内容精彩!学到很多
59