Br J Cancer:计算机断层扫描(CT)相比于胸透(CXR)在妊娠滋养细胞瘤形成的初步评估中并无优势
2020-12-29 xiaozeng MedSci原创
妊娠滋养细胞肿瘤(GTN)通常采用国际妇产科联合会(FIGO)评分系统进行分类,以鉴定患者属于单药化疗耐药(SACR)的低风险(得分≤6)或高风险(得分≥7)。
妊娠滋养细胞肿瘤(GTN)通常采用国际妇产科联合会(FIGO)评分系统进行分类,以鉴定患者属于单药化疗耐药(SACR)的低风险(得分≤6)或高风险(得分≥7)。
FIGO评分系统通常使用胸部X光片(CXR)方式作为评估肿瘤肺转移的标准。计算机断层扫描(CT)在检测肺转移方面相比于胸部X光片(CXR)检测具有更高的敏感性,但目前尚不清楚其对患者结局的影响。
箱形图比较基于CXR和CT的肺转移成像的FIGO得分
在该研究中,共有589名进行GTN评估的患者同时接受了CXR和CT检查。患者的治疗决策主要基于CXR。研究人员比较了CXR和CT检测的患者的转移次数、风险评分和风险类别。相比于患者的预后情况、SACR的发生率、TNhCG(正常绒毛膜促性腺激素)达到正常的时间和原发化疗耐药性(PCR),CT相关的胸部评分被评估为影响治疗决策的主要因素。
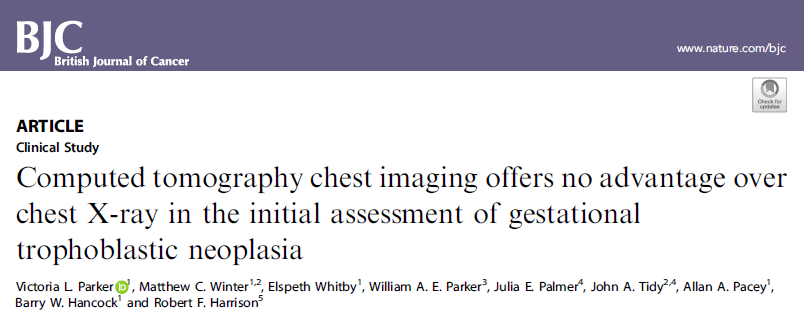
相关治疗结果流程图
该研究结果显示,相比于CXR,CT的转移检测和FIGO评分更高。 在188例(31.9%)患者中CT检测的FIGO评分更高,其中的43例从低风险被重新分类为高风险,而其中的23例患者(53.5%)接受了治愈性单药化疗。当评分或风险组改变时,SACR发生率更高。 CXR检测的转移而非CT检测的能够延长TNhCG时间。逻辑回归分析显示,在预测PCR时,CXR与CT之间没有差异。
综上,该研究结果显示,CT能够将改善患者的SACR预测,但并不影响总体的治疗结果、TNhCG或PCR的预测。而由于较低的辐射剂量以及成本的问题,研究人员建议继续使用基于CXR的评估策略。
原始出处:
Parker, V.L., Winter, M.C., Whitby, E. et al. Computed tomography chest imaging offers no advantage over chest X-ray in the initial assessment of gestational trophoblastic neoplasia. Br J Cancer (16 December 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#计算机#
32
#初步评估#
35
#细胞瘤#
33
这个新
81
很好的文章,认真学习
81
学习学习了
97