European Radiology:使用氧提取分数(OEF)评价子痫前期患者深部灰质的脑氧代谢变化
2022-08-06 shaosai MedSci原创
氧提取分数(OEF)是脑组织活力和功能的一个重要指标,利用平扫MRI绘制其图谱具有很大的临床意义。
 包括慢性高血压、妊娠期高血压和先兆子痫(PE)等高血压疾病影响着全世界多达10%的孕妇,是孕产妇死亡的六大原因之一,占所有孕产妇死亡的近10%。
包括慢性高血压、妊娠期高血压和先兆子痫(PE)等高血压疾病影响着全世界多达10%的孕妇,是孕产妇死亡的六大原因之一,占所有孕产妇死亡的近10%。
PE患者可有多种神经系统症状,与系统性血管损伤、内皮功能紊乱以及随之而来的低灌注和缺氧有关。然而,目前还没有一种方法可以直接测量孕妇大脑中的氧代谢情况。诊断PE最常用的方法是经颅多普勒超声(TCD),但由于TCD只能用于评估大动脉,无法反映脑内微循环的变化。磁共振成像(MRI)可以获得形态学和生理学信息。最近,体外非相干运动(IVIM)已被用于评估PE患者的灌注分数和水肿。IVIM可以估计毛细血管水平的血液灌注,但不能直接反映大脑的氧代谢。因此,迫切需要找到一个精确而敏感的神经影像学标志物来直接评估PE患者的脑氧代谢情况。
氧提取分数(OEF)是脑组织活力和功能的一个重要指标,利用平扫MRI绘制其图谱具有很大的临床意义。QSM和基于血氧水平的量化幅度(QSM + qBOLD = QQ)的OEF图谱是一种新的MRI技术,能够无创地量化脑氧代谢。
近日,发表在European Radiology杂志的一项研究比较了先兆子痫患者、健康孕妇和非怀孕育龄妇女的深层灰质(GM)的OEF值,探讨了他们在GM中的脑氧代谢差异,为临床早期识别潜在的中枢神经系统损伤,并进行有针对性的治疗以减少PE和随之而来子痫并发症的发生提供了参考依据。
本研究纳入47名PE患者、40名NPHCs和21名PHCs。脑部OEF值由QSM和基于定量血氧水平的幅度(QSM + qBOLD = QQ)图谱计算得出。采用单因素方差分析来比较三组的平均OEF值。使用接ROC曲线分析估计每个感兴趣区域的平均OEF值的曲线下面积。
本研究发现,丘脑、壳核、尾状核、苍白球和黑质的平均OEF值在这三组中有明显差异(F=5.867,p=0.004;F=5.142,p=0007;F=6.158,p=0.003;F=6.319,p=0.003;F=5.491,p=0.005)。这5个区域的平均OEF值在PE患者中高于NPHCs和PHCs(P < 0.05)。这些ROI的AUC从0.673到0.692(p < 0.01),截断值从35.1到36.6%不等,表明OEF值可以区分PE患者和非PE患者。逐步多变量分析显示,OEF值与孕妇的血细胞比容相关(r = 0.353,p = 0.003)。
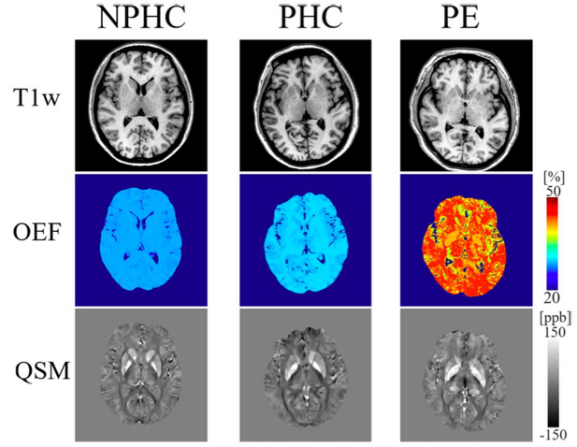
图 来自NPHC、PHC和PE的代表性T1w、OEF、QSM maps。T1w和QSM maps可以准确识别解剖结构。丘脑、壳核、尾状核、苍白球和黑质的平均OEF值在三组中明显不同。与NPHC和PHC相比,PE患者的平均OEF值更高,但NPHC和PHC之间的平均OEF值没有统计学上的显著差异。NPHC,34岁;PHC,33岁,35孕周;PE,30岁,33孕周
本研究发现,与PHCs和NPHCs相比,PE患者的丘脑、壳核、尾状核、苍白球和黑质的平均OEF值增加,这些变化可能是克服严重缺氧和维持脑氧代谢的一种补偿机制。可以使用基于QQ的无创OEF图谱来测量孕妇大脑中OEF值的明显变化,较高的平均OEF值常预示着高血压疾病的存在。
原文出处:
Linfeng Yang,Junghun Cho,Tao Chen,et al.Oxygen extraction fraction (OEF) assesses cerebral oxygen metabolism of deep gray matter in patients with pre-eclampsia.DOI:10.1007/s00330-022-08713-7
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
35
#代谢变化#
39
学习
36
#子痫前期#
37
#评价#
51