J Oral Pathol Med:口服补充剂可降低癌症患者的口腔黏膜炎发生率及严重性
2020-08-20 MedSci原创 MedSci原创
本次系统回顾和荟萃分析旨在评估口服补充剂对接受化疗和/或放疗的癌症患者口腔黏膜炎的治疗效果。
本次系统回顾和荟萃分析旨在评估口服补充剂对接受化疗和/或放疗的癌症患者口腔黏膜炎的治疗效果。

研究人员在6个数据库和灰色文献中进行了搜索。通过Cochrane协作风险偏倚工具评估纳入研究的方法学,通过GRADE工具评估证据质量。
结果,共纳入12项随机临床试验。采用的口服补充剂是含有氨基酸和矿物质(元素),谷氨酰胺和锌的口服元素饮食。大多数研究显示,在接受放化疗的患者中,使用谷氨酰胺和锌可延缓OM的发生,使用谷氨酰胺、锌和矿物质可降低OM的严重程度。荟萃分析显示,锌组发生口腔黏膜炎的风险略低于对照组(RR:0.71,95%CI:0.53-0.96,P=0.02,n=982),而谷氨酰胺组呈现与对照组相同的风险(RR:0.91,95%CI:0.78-1.05,P=0.19,n=314)。证据质量表明,锌和谷氨酰胺研究从评估的结果中估计效果的信心较低。
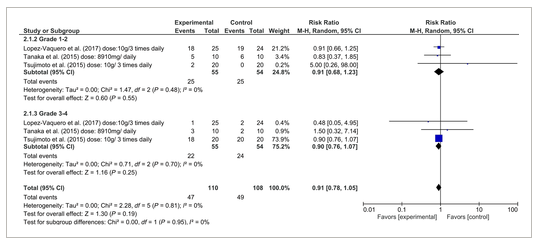
综上所述,锌是治疗口腔黏膜炎的一个有希望的策略,因为它延迟了口腔黏膜炎的发生并降低了其严重程度。另一方面,谷氨酰胺和矿物质在预防和/或治疗癌症患者口腔黏膜炎方面没有强有力的证据。
原始出处:
Amanda Gomes de Menêses, Ana Gabriela Costa Normando, et al., Effects of oral supplementation in the management of oral mucositis in cancer patients: A meta-analysis of randomized clinical trials. J Oral Pathol Med. 2020 Feb;49(2):117-125. doi: 10.1111/jop.12901.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#黏膜炎#
42
#发生率#
33
#Pathol#
48
#Oral#
44
#严重性#
41
#癌症患者#
35
#黏膜#
41
#Med#
36