Science:肿瘤免疫治疗效果不同的原因被揭示
2016-03-04 MedSci MedSci原创
一项最新研究指出肿瘤新抗原(tumor neoantigens)能帮助医师们了解癌症患者对癌症免疫疗法的应答情况,这将为实现个体化癌症治疗铺平道路。这一研究成果公布在3月3日的Science杂志上。 在过去的几年中,癌症免疫疗法变得越来越热门,从最开始发现我们的免疫系统能抑制癌症生长,到后来发现癌细胞中免疫机制的多重作用,再到目前陆续跟进的临床实验,癌症免疫疗法争论不休,同时也成果不断。
一项最新研究指出肿瘤新抗原(tumor neoantigens)能帮助医师们了解癌症患者对癌症免疫疗法的应答情况,这将为实现个体化癌症治疗铺平道路。这一研究成果公布在3月3日的Science杂志上。
在过去的几年中,癌症免疫疗法变得越来越热门,从最开始发现我们的免疫系统能抑制癌症生长,到后来发现癌细胞中免疫机制的多重作用,再到目前陆续跟进的临床实验,癌症免疫疗法争论不休,同时也成果不断。然而在临床上只有20%的患者会对这些治疗方法产生应答,因此科学家们亟待了解成功应答背后的因素。
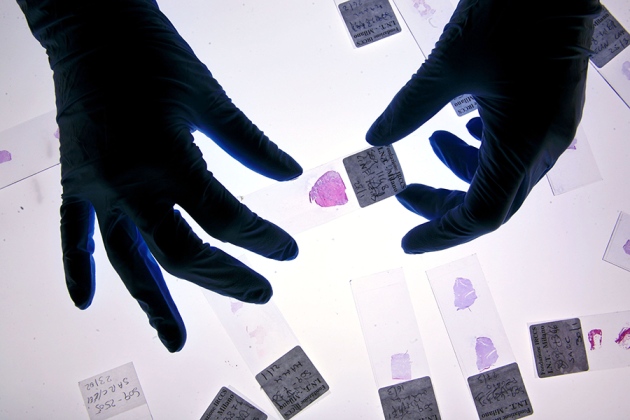
其中一个因素就是所谓的“neoantigens(新抗原)”,新抗原就是肿瘤中的突变多肽,在正常组织中是不存在的。对应于不同的突变,这些新抗原也会表现出肿瘤内异质性,其中一些属于一级克隆(所有肿瘤细胞中都有),还有一些是亚克隆(只存在于一部分细胞中)。
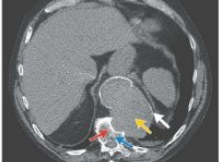
在最新这篇文章中,研究人员分析了肺癌和恶性黑色素瘤,发现肿瘤新抗原与患者生存力提高,肿瘤浸润性淋巴细胞(Tumor infiltrating lymphocytes)增多,以及免疫治疗应答延长有关。
这为预测患者对免疫疗法的应答提出了一个潜在的生物标记物,而且区分克隆与亚克隆新抗原也有助于识别哪种新抗原最有效,能靶向不同类型的治疗方法。循环中CD8+PD-1+淋巴细胞可能是其中的关键,最近多篇研究证实了这一点。
原始出处:
Nicholas McGranahan,et al.Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade.Science 03 Mar 2016: pp. DOI: 10.1126/science.aaf1490
Gros A, Parkhurst MR, Tran E, Pasetto A, Robbins PF, Ilyas S, Prickett TD, Gartner JJ, Crystal JS, Roberts IM, Trebska-McGowan K, Wunderlich JR, Yang JC, Rosenberg SA.Prospective identification of neoantigen-specific lymphocytes in the peripheral blood of melanoma patients. Nat Med. 2016 Feb 22. doi: 10.1038/nm.4051.
Ward JP, Gubin MM, Schreiber RD.The Role of Neoantigens in Naturally Occurring and Therapeutically Induced Immune Responses to Cancer.Adv Immunol. 2016;130:25-74
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#治疗效果#
22
免疫方面东西太复杂了
134
哪种新抗原最有效,能靶向不同类型的治疗方法。
120
高大上的研究
105
#SCIE#
24
难懂,好好学习
84
继续努力
99
什么跟什么?_?
123
题目大了点
55