SCIENCE:肿瘤转移至淋巴结需要YAP依赖性代谢适应
2019-02-10 海北 MedSci原创
在癌症患者中,肿瘤向前哨淋巴结(LN)的转移预测着疾病的进展,并且经常指导治疗决策。
在癌症患者中,肿瘤向前哨淋巴结(LN)的转移预测着疾病的进展,并且经常指导治疗决策。
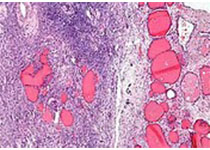
至今为止,我们关于肿瘤LN转移的潜在机制知之甚少。最近,通过使用小鼠原发性和LN转移性肿瘤的比较转录组学和代谢组学分析,研究人员发现,LN转移需要肿瘤细胞经历向脂肪酸氧化的代谢转变(FAO)。转录共激活因子相关蛋白(YAP)在LN转移性肿瘤中被选择性激活,导致FAO信号传导途径中基因的上调。
对FAO的药理学抑制或YAP的遗传消除抑制了小鼠肿瘤的LN转移。几种生物活性胆汁酸在转移性LN中积累到高水平,并且这些胆汁酸可能通过核维生素D受体激活肿瘤细胞中的YAP。
因此,该结果显示,抑制FAO或YAP可能可以作为减轻肿瘤转移至LN的潜在治疗策略。
原始出处:
Choong-kun Lee et al. Tumor metastasis to lymph nodes requires YAP-dependent metabolic adaptation. SCIENCE, 2019; doi: 10.1126/science.aav0173
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#YAP#
26
#肿瘤转移#
55
#淋巴结#
26
#SCIE#
22