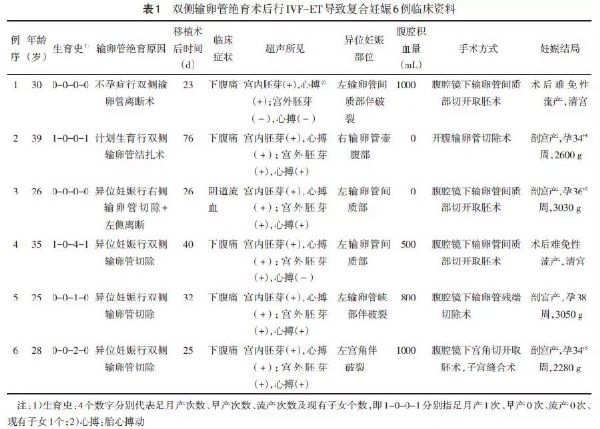
双侧输卵管绝育术后行体外受精-胚胎移植导致复合妊娠6例
2018-12-04 黄宝友 赵红琴 金武敏 中国实用妇科与产科杂志
复合妊娠(heterotopic pregnancy,HP)是指胚胎同时在2个或2个以上部位植入,其中至少1个属于宫内妊娠,其余属于异位妊娠,即宫内妊娠和异位妊娠同时存在。正常情况下,自然妊娠发生HP的发生率极低约1/30 000,随着体外受精-胚胎移植(in vitro fertilization-embryo transfer,IVF-ET)等辅助生殖技术的日益发展,HP发生率高达1%~11%
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#绝育术#
23
#输卵管#
34
#胚胎#
28
#胚胎移植#
39
#双侧#
34
#受精#
30
学习了
85