PNAS:西安交大在自然杀伤细胞调控肺癌免疫方面取得新突破
2018-12-06 佚名 西安交大新闻网
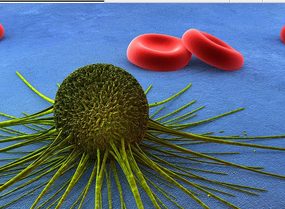
自然杀伤(NK)细胞与主要组织相容性I类分子(MHC-I)的相互作用在肿瘤免疫中起重要作用,NK细胞通过与MHC-I类分子相互作用而获得“教育”(education),成为“授权”(licensed)的NK细胞,“授权”的NK细胞具有增强杀伤靶细胞的能力,在肿瘤的发生、发展中具有重要作用。NK细胞与肺癌的易感性及耐药性密切相关,但NK细胞介导的清除肺癌的机制仍不清楚。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PNAS#
32
#西安交大#
30
#新突破#
25
#自然杀伤细胞#
47