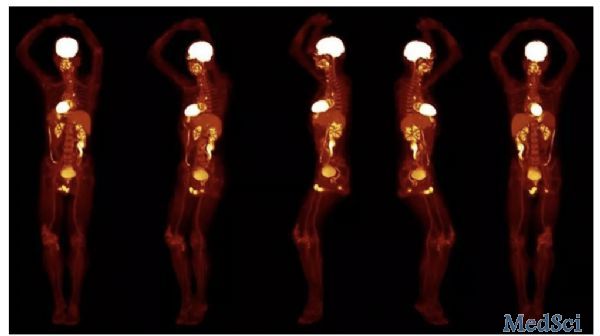
黑科技!20秒全身3D成像的PET扫描仪来了
2019-06-23 Nature自然科研 Nature自然科研
一款最新的医学成像设备只需20秒就能完成全身3D扫描,不久或将在研究和临床领域得到广泛应用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
25
#PET扫描#
41
#PET#
33
#3D#
27
666
74