Hepatology:胆汁性肾病引起急性肾衰竭同时伴有集合管中水通道蛋白2表达缺失
2019-01-31 邵玥明,温晓玉 临床肝胆病杂志
肾功能损伤常发生于肝病患者中。肝肾综合征是引起肝硬化患者急性肾损伤(AKI)的重要原因(HRS-AKI,1型)。除此之外,以胆汁性肾病最为常见,其特征是胆管内胆汁管型和胆管损伤。由于胆汁性肾病患者的资料主要来自病例报告或尸检研究,本研究目的是探究胆汁性肾病的发病率和临床过程。
肾功能损伤常发生于肝病患者中。肝肾综合征是引起肝硬化患者急性肾损伤(AKI)的重要原因(HRS-AKI,1型)。除此之外,以胆汁性肾病最为常见,其特征是胆管内胆汁管型和胆管损伤。由于胆汁性肾病患者的资料主要来自病例报告或尸检研究,本研究目的是探究胆汁性肾病的发病率和临床过程。
选取2000年-2016年在胃肠内科、肝病科或内分泌科住院并接受肾活检的149例患者作为研究对象。其中,79例患者有肝病史和肾功能恶化。
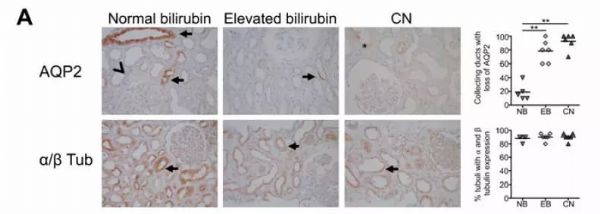
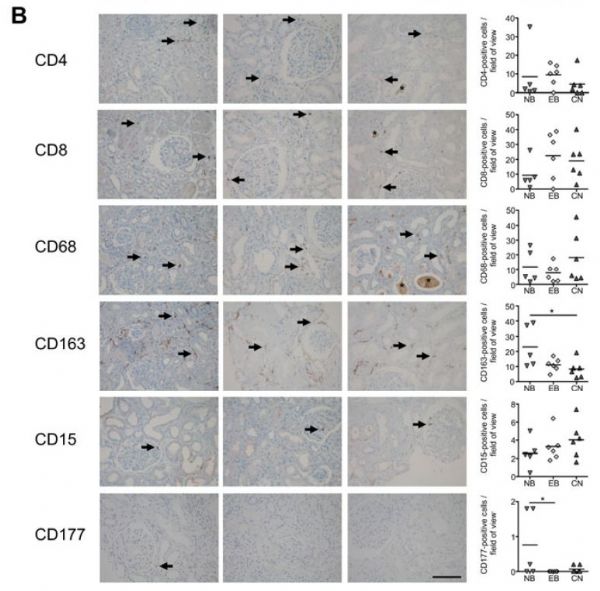
根据最新的EASL标准,79例患者中急性肾损伤45例(57%),慢性肾病34例(43%)。其中45例急性肾损伤患者中肾活检示:8例(17.8%)诊断为胆汁性肾病,而慢性肾病患者均未被诊断为胆汁性肾病。单变量分析发现,血清胆红素、碱性磷酸酶、尿胆红素和尿胆素原可作为诊断胆汁性肾病的预测因素。与胆红素正常的急性肾损伤患者相比,高胆红素血症和胆汁性肾病患者的组织学分析显示,集合管中发生了水通道蛋白2(AQP2)表达缺失。79例患者中的4例发生了需要进行医疗干预的活检相关并发症(5.1%)。
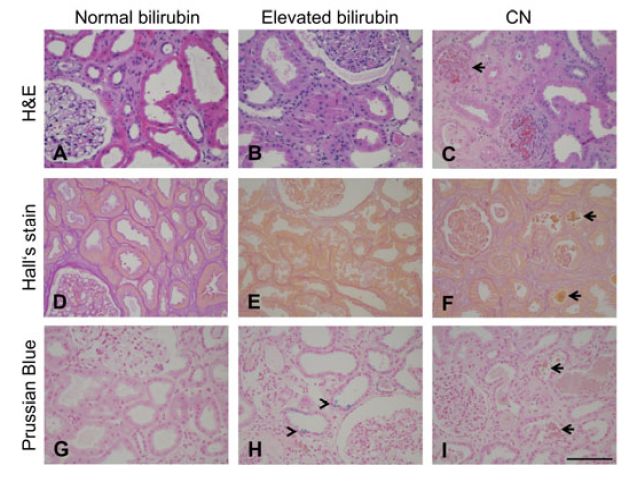
总之,胆汁性肾病常发生于肝病,急性肾损伤和高胆红素患者中。高胆红素血症和胆汁性肾病患者中AQP2的丢失可能是胆汁淤积的毒性作用的结果,并且是肾功能损害的部分原因。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#集合管#
31
#胆汁性#
27
#肾衰竭#
33
#EPA#
23
#胆汁#
48
不错的作品,为我们探讨研究提供了方针,必须给点个赞了!
46