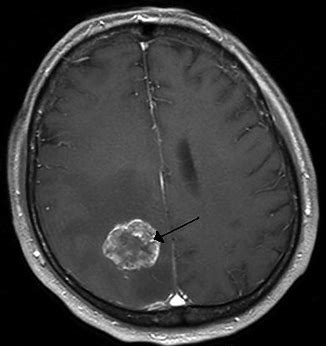
脑肿瘤一线治疗:VAL-083的II期临床试验即将开始
2020-02-20 Allan MedSci原创
DelMar是一家专注于开发实体瘤癌症疗法的生物制药公司,近日宣布已注册并开始VAL-083的II期临床研究,VAL-083旨在一线治疗MGMT未甲基化的胶质母细胞瘤(GBM)。
DelMar是一家专注于开发实体瘤癌症疗法的生物制药公司,近日宣布已注册并开始VAL-083的II期临床研究,VAL-083旨在一线治疗MGMT未甲基化的胶质母细胞瘤(GBM)。该试验正在中国广州的中山大学癌症中心(SYSUCC)进行,计划招募多达30例患者,以确定VAL-083能否改善GBM患者的无进展生存期(PFS)。
DNA修复蛋白O6-甲基鸟嘌呤-DNA甲基转移酶(O6-methylguanine-DNA methyltransferase,MGMT)启动子甲基化是胶质瘤患者的重要分子标志物,与胶质瘤预后及烷化剂耐药有关。而对于MGMT未甲基化的胶质母细胞瘤(GBM),其MGMT基因的转录水平较高,理论上,此类患者对烷化剂耐药程度较高,亟需新型药物。VAL-083(二氢半乳糖醇)是一种双功能DNA靶向剂,可在鸟嘌呤的N7位引入链间DNA交联,导致DNA双链断裂和癌细胞死亡。
原始出处:
https://www.firstwordpharma.com/node/1702095?tsid=4
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#I期临床试验#
46
#I期临床#
58
#II期临床试验#
54
#脑肿瘤#
43
#II期临床#
48