J Thromb Haemost:血浆中甘露糖结合凝集素水平与静脉血栓栓塞风险
2019-06-23 xing.T MedSci原创
由此可见,该研究结果表明低血浆MBL水平与VTE风险降低有关,特别是DVT风险降低。
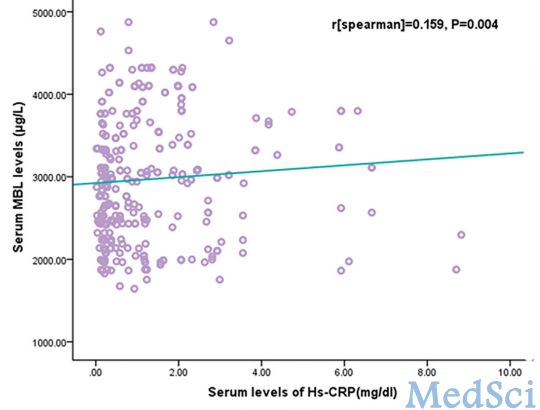
动物和观察研究表明补体在静脉血栓栓塞(VTE)中发挥病理生理学作用,但初始机制尚不清楚。与改变的宿主细胞结合的甘露糖结合凝集素(MBL)导致凝集素补体途径的激活,并且较高和较低MBL水平都与心血管疾病的病理生理学机制有关。近日,血栓和凝血疾病权威杂志Journal of Thrombosis and Haemostasis上发表了一篇研究文章,其旨在调查血浆MBL水平与未来VTE事件风险之间的关系。
研究人员对417名VTE患者进行了巢式病例对照研究,并对849名来自一般人群的年龄和性别匹配的对照者进行了研究(特罗姆瑟研究)。研究人员使用ELISA测量血浆MBL水平。Logistic回归模型用于估计VTE在血浆MBL水平四分位数个体中的比值比(OR)。
在多变量调整后,血浆MBL水平处于最高四分位数(≥2423ng/mL)的受试者相比,血浆MBL水平处于最低四分位数(<435ng/mL)的受试者整体VTE(OR为0.79,95%CI:0.56-1.10)和深静脉血栓形成(DVT)的OR降低(OR为0.70,95%CI:0.47-1.04)。对于VTE、DVT和肺栓塞(PE),ORs随血液采样和VTE事件之间的间隔时间缩短而显著降低。
由此可见,该研究结果表明低血浆MBL水平与VTE风险降低有关,特别是DVT风险降低。
原始出处:
Robin Amanda Liang.et al.Plasma Levels of Mannose‐Binding Lectin and Future Risk of Venous Thromboembolism.Journal of Thrombosis and Haemostasis.2019.https://doi.org/10.1111/jth.14539
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#HAE#
35
#静脉血栓栓塞风险#
37
#静脉血#
31
#甘露糖结合凝集素#
27
#静脉#
21
学习了
73