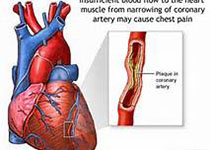
Circulation:微囊蛋白1(Cav1)通过抑制低密度脂蛋白转运和内皮细胞炎症发挥抗动脉粥样硬化作用
2019-07-18 MedSci MedSci原创
动脉粥样硬化是由病理、生理、炎症和脂质代谢因子协同作用导致的。研究表明,高脂血症小鼠缺失微囊蛋白1(Cav1)/质膜微囊会强烈抑制动脉粥样硬化,这归因为内皮NO合酶(eNOS)激活、NO生成增加以及炎症和低密度脂蛋白转运减少。但eNOS激活和NO产生在Cav1动脉粥样硬化中的保护作用以及Cav1/质膜微囊控制饮食诱导的动脉粥样硬化的分子机制尚不清楚。研究人员建立了eNOS、Cav1和Ldlr三敲除
动脉粥样硬化是由病理、生理、炎症和脂质代谢因子协同作用导致的。研究表明,高脂血症小鼠缺失微囊蛋白1(Cav1)/质膜微囊会强烈抑制动脉粥样硬化,这归因为内皮NO合酶(eNOS)激活、NO生成增加以及炎症和低密度脂蛋白转运减少。但eNOS激活和NO产生在Cav1动脉粥样硬化中的保护作用以及Cav1/质膜微囊控制饮食诱导的动脉粥样硬化的分子机制尚不清楚。
研究人员建立了eNOS、Cav1和Ldlr三敲除小鼠来研究NO产生在Cav1依赖性动脉粥样硬化保护功能中的作用。
研究结果显示,Cav1缺乏会显著抑制Ldlr-/-eNOS-/-小鼠发生动脉粥样硬化,表明动脉粥样硬化抑制与NO合成增多无关。相反,Cav1/质膜微囊缺失会抑制低密度脂蛋白跨内皮细胞转运、促动脉粥样硬化纤维连接蛋白沉积,并干扰血流介导的内皮细胞炎症。
与Cav1/质膜微囊可能是在血流依赖的炎症早期发挥作用的观点一致,在主动脉弓动脉粥样硬化易发区和动脉粥样硬化耐药区也观察到了不同的Cav1表达和质膜微囊分布图谱,即使是在野生小鼠中,也可观察到类似现象。
综上所述,本研究揭示了Cav1/质膜微囊作为动脉粥样硬化的中心调控因子的作用,它不依赖内皮细胞eNOS激活和NO产生,将生物力学、代谢和炎症通路联系起来。
原始出处:
Cristina M. Ramírez,et al.Caveolin-1 Regulates Atherogenesis by Attenuating Low-Density Lipoprotein Transcytosis and Vascular Inflammation Independently of Endothelial Nitric Oxide Synthase Activation.https://doi.org/10.1161/CIRCULATIONAHA.118.038571Circulation. 2019;140:225–239
本文系梅斯医学(MedSci)原创编译,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#转运#
40
#Cav1#
36
#细胞炎症#
46
#粥样硬化#
45
#脂蛋白#
31
学习
63