NEJM:社区干预措施使收缩压多下降5 mmHg!预计降低30%心血管病死亡和残疾
2020-02-21 xujing 中国循环杂志
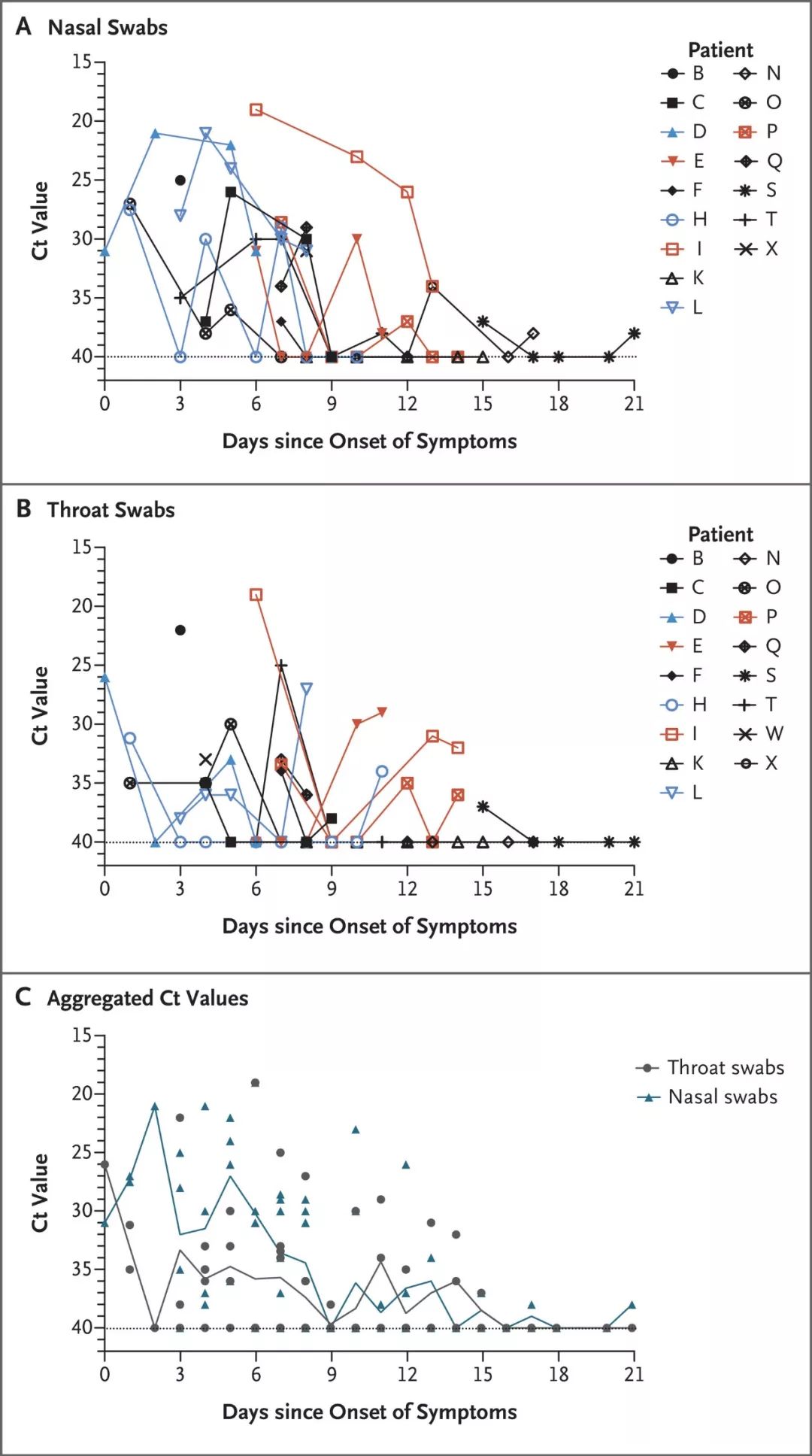
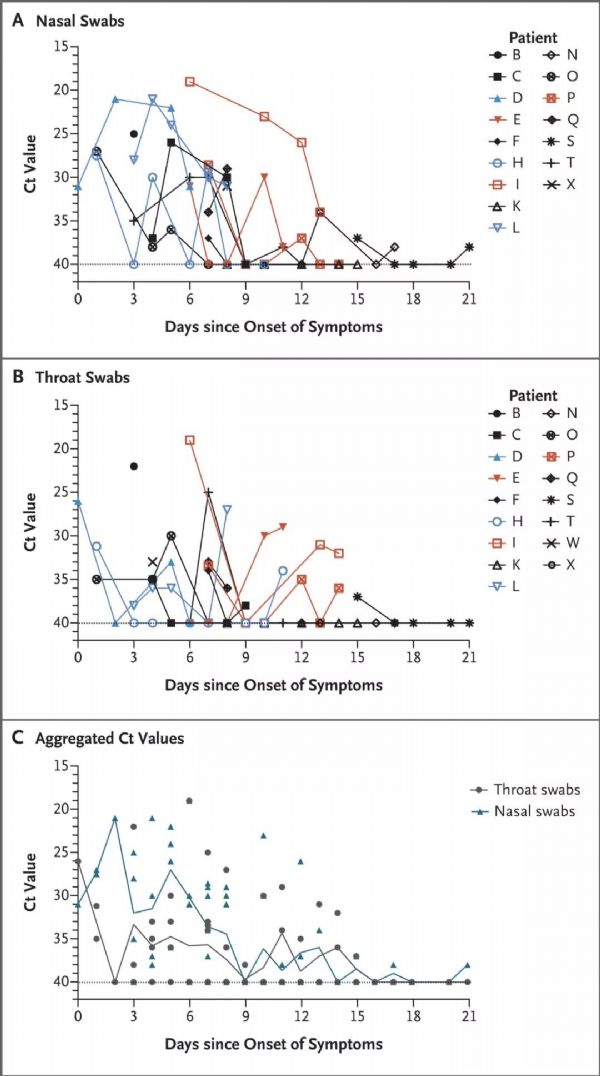
新英格兰医学在刊登的一项亚洲三国社区高血压干预效果研究发现,社区医护人员主导的可持续、低成本的干预措施使高血压患者的治疗依从性更佳,平均收缩压多降低了5 mmHg,提高了血压达标率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血管病#
82
#收缩压#
41
#干预措施#
0
#社区#
0
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
55