Cell Metab:节食有道,神经元阀门帮你管住嘴
2020-01-21 Reduction C 转化医学网
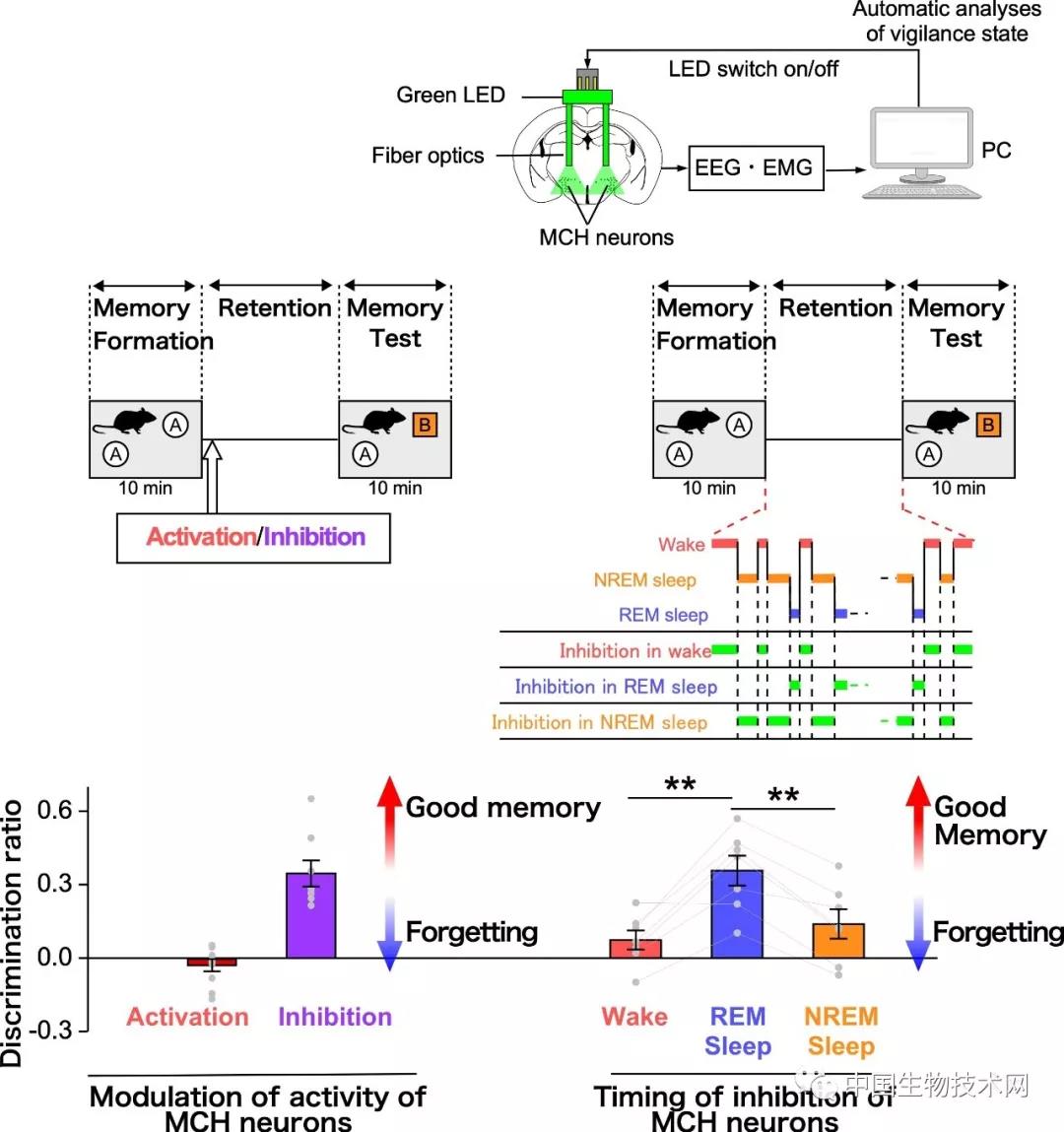
导 读:你是否曾经在吃过某种食物后恶心反胃,之后一旦看到它就失去食欲?这是因为胃肠道向大脑产生了一种信号让你产生这种恶心感。传统观点认为大脑中存在一种来自胃肠道的回路能够帮助抑制食欲,一旦被过度激活就会使你产生不适。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#MET#
33
#CEL#
28
#Cell#
34
#Meta#
45
#节食#
46