Blood:Fc-修饰型抗PF4-NET复合物单克隆抗体KKO明显改善脓毒症预后
2019-11-15 QQY MedSci原创
脓毒症是由感染引起的全身炎症反应综合征,特征是炎症导致多器官系统功能障碍。发病率和病死率高,需要改善其治疗方法。中性粒细胞在脓毒症过程中具有至关重要的作用,它释放由组蛋白和有毒抗菌蛋白组成的胞外中性粒细胞陷阱(NETs)来捕捉病原体,但与此同时也会损伤宿主组织。发病时,患者往往已有很重的NET负荷,导致多器官受损。因此,发病时再予以抑制NET释放的干预措施,在预防NET相关损伤方面可能是无效的。加
PF4通过稳定NETs和增强NET介导的微生物诱捕来改善脓毒症的预后
KKO,一种Fc修饰的HIT样抗体,可进一步加强PF4在脓毒症中的有利作用
摘要:
脓毒症是由感染引起的全身炎症反应综合征,特征是炎症导致多器官系统功能障碍。发病率和病死率高,需要改善其治疗方法。中性粒细胞在脓毒症过程中具有至关重要的作用,它释放由组蛋白和有毒抗菌蛋白组成的胞外中性粒细胞陷阱(NETs)来捕捉病原体,但与此同时也会损伤宿主组织。发病时,患者往往已有很重的NET负荷,导致多器官受损。因此,发病时再予以抑制NET释放的干预措施,在预防NET相关损伤方面可能是无效的。加强NET降解可能会释放捕获的细菌和有毒的NET降解产物(NDPs),而且可能也没有多少治疗效果。
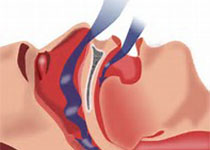
Gollomp等人认为稳定NETs和隔离NDPs或可加强脓毒症的治疗,并经研究发现血小板因子4(PF4),一种血小板相关的趋化因子,可结合NETs,并使其更为紧密,从而增强其对脱氧核糖核酸酶I的抵抗力。此外,研究人员还发现PF4可增强NET介导的细菌捕获,减少NDPs的释放,提高脓毒症小鼠模型的预后。
因此,研究人员开发了一种Fc-修饰的KKO,不会诱导任何负性预后。采用这种抗体治疗可放大PF4的效应,减少NDP释放和细菌扩散,提高脓毒症小鼠模型的存活。综上所述,本研究表明该新型的靶向NET的治疗方法或可用于改善脓毒症患者预后。
原始出处:
Kandace Gollomp, et al.Understanding how Fc-modification transforms a pathogenic HIT-like monoclonal antibody into a novel treatment for sepsis.blood.2019002329.https://doi.org/10.1182/blood.2019002329
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#克隆#
0
#PF4#
46
#复合物#
44
#NET#
34
#修饰#
25