ADA 2019:肾脏与心血管并发症有何关系?如何影响糖尿病治疗和预后?
2019-06-16 国际糖尿病编辑部 国际糖尿病
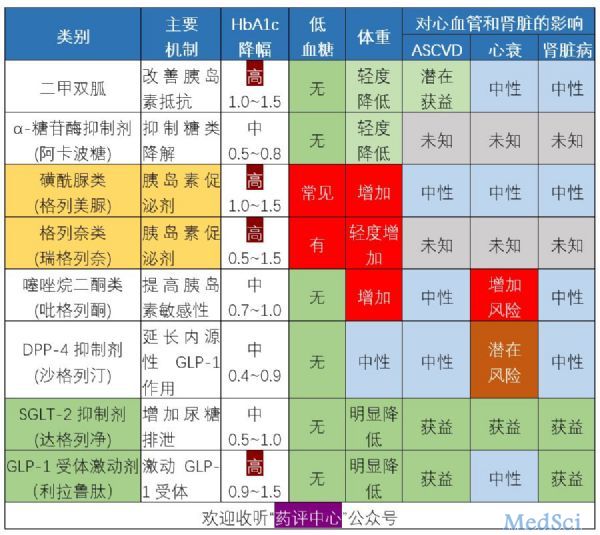
编者按:众所周知,糖尿病患者中肾脏及心血管并发症常伴发存在。那么,肾脏疾病与心血管并发症之间到底存在着怎样的相互关系?相关研究取得了哪些重大进展?针对糖尿病患者,我们应如何进行心肾并发症的有效防治?在第79届ADA科学年会上,Edwin Bierman奖得主——丹麦哥本哈根大学Peter Rossing教授就上述临床实践中大家所关心的现实问题进行了专题解析。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#并发#
37
#糖尿病治疗#
49
#ADA#
32
#心血管并发症#
51
#血管并发症#
38
谢谢MedSci提供最新的资讯
33